
A breast cancer diagnosis can bring lots of information and be difficult to understand at first. Here is a guide to help you come to terms with the information about the different types and features of breast cancer, so you can understand your diagnosis better.
Put very simply, breast cancer happens when cells in the breast tissue grow uncontrollably, forming a tumour1.
Anatomy of the breast
It helps to understand the anatomy of the breast and the area around it to understand your breast cancer diagnosis. The breasts are made up of fat, glandular tissue divided into lobes, milk ducts and connective tissue2. In adult women, breasts respond to changes in hormone levels and can produce milk. In each breast there are around 15-20 sections called lobes. Each lobe is made up of smaller structures called lobules3. Small glands at the end of each lobule are where the milk is produced. The lobes, lobules and milk glands are all connected via ducts, which deliver milk to the nipple openings3.
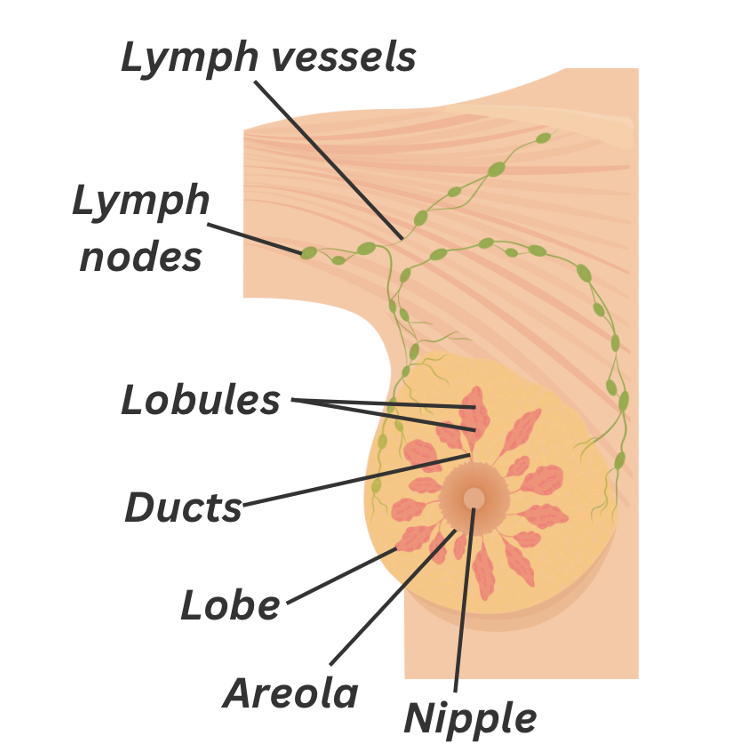
Figure 1. The anatomy of the breast
Around the breast, there are bean-shaped nodes called lymph nodes. They are found in groups along lymph vessels. The lymph nodes are part of the lymphatic system, which drains lymph fluid containing waste from tissues and organs in the body. They are responsible for filtering, storing and releasing lymph fluid. This helps to keep the fluid levels balanced and defend the body from disease and infection.
Types of Breast Cancer
Most breast cancer tumours start in the milk ducts or the lobules. The location of the tumour is important for diagnosis, as the type of the breast cancer depends on where in the breast the tumour formed.
In situ (non-invasive) breast cancer
In situ, also known as non-invasive, means that the cancer is not currently able to spread beyond the tissue where it first started. There are two main types:
1. Ductal carcinoma in situ (DCIS)
Around 20% of new cases of breast cancer are DCIS, this is when breast cancer cells that have developed inside the milk ducts have not spread into the surrounding breast tissue or to other parts of the body4. If left untreated, DCIS could potentially develop into invasive breast cancer.
2. Lobular carcinoma in situ (LCIS)
This is a non-harmful benign breast condition that is not considered breast cancer. LCIS develops in the lobules and can increase the risk of developing breast cancer.
Invasive breast cancer
Invasive, also known as infiltrating, no special type (NST) or not otherwise specified (NOS) breast cancer, is when the cancer cells have spread into nearby breast tissue. Most breast cancers are considered invasive. There are two main types of invasive breast cancer:
1. Invasive ductal carcinoma (IDC)
This type of breast cancer starts in the cells lining the milk ducts and accounts for approximately 80% of all cases of invasive breast cancer5.
2. Invasive lobular carcinoma (ILC)
This starts in the lobules and accounts for around 10% of all cases of invasive breast cancer5. Research suggests that around 20% of women diagnosed with ILC have cancer in both of their breasts.
These are the most common types of invasive breast cancers, but there are rarer types, such as:
- Inflammatory breast cancer: Accounts for 1-5% of breast cancers6. Can be seen in either the ducts or lobules and is a fast-growing type of invasive breast cancer6,7. It is called ‘inflammatory’ as it causes abnormal swelling and redness, appearing as a breast infection. For this reason, it can often be misdiagnosed as an infection6.
- Paget’s disease: Paget’s disease, also known as Paget’s disease of the nipple is a rare type of breast cancer6. It accounts for 1-4% of patients and is commonly diagnosed alongside another more common breast cancer type. It is characterised by abnormal cells, known as Paget cells, forming on the skin of the nipple and the areola.
- Phyllodes tumours: These are a rare subtype of breast cancer that develops out of the connective tissue in the breast, commonly affecting women in their 40s and those with Li-Fraumeni syndrome6. Only around 25% of these tumours are cancerous.
- Angiosarcoma of the breast: Originates in the lining of the lymph or blood vessels6. It is a fast-growing cancer that is most common in those over the age of 70, although it can develop at any age. A lot of the time, breast angiosarcomas can go undiagnosed until they are fairly advanced.
Other rare invasive breast tumour subtypes include low-grade adenosquamous carcinoma, adenoid cystic carcinoma, mucinous carcinoma, papillary carcinoma, medullary carcinoma, and tubular carcinoma.
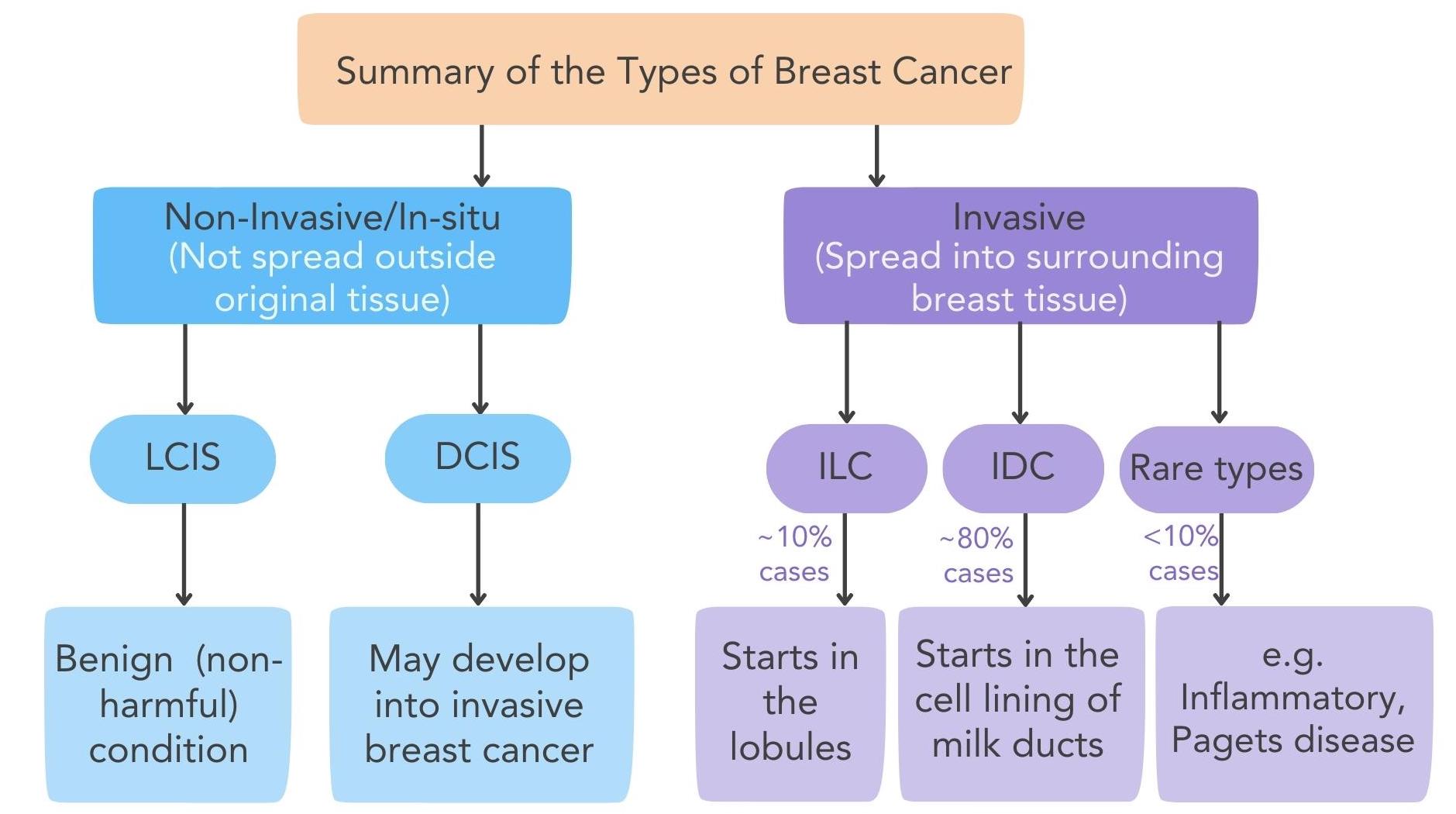
Figure 2. The different types of non-invasive/in-situ and invasive breast cancer
What is Breast Cancer grading?
Breast cancer grading, also known as differentiation, gives cancer cells a grade according to similar they look to normal cells in the body. The more that cancer cells look like normal cells, the more differentiated they are. To determine a grade ranging from 1-3 a pathologist examines a tumour sample to check:
- How similar the cancer cells are to healthy cells
- How many and how fast the cancer cells are dividing
Breast cancer grades
Grade 1 cancer cells:
- Look similar to healthy breast cells
- Grow and divide slowly
- Are well differentiated
- Are arranged in the expected structure
Grade 2 cancer cells:
- Looking less similar to healthy cells
- Are often larger and show variation in shape and size
- Grow and spread faster than healthy cells
- Are moderately differentiated – have more abnormal features than grade 1 cells
Grade 3 cancer cells:
- Look abnormal
- May grow or spread faster
- Are poorly differentiated – have more abnormal features
What is Breast Cancer staging?
Breast cancer stage is calculated through considering the size of the tumour, spread to lymph nodes, how different cancer cells look compared to healthy cells, and information gathered through other tests. Stages range 0-4:
Stage 0
Cancer is non-invasive and has not spread to other tissues. Can also be called in situ and concerns LCIS and DCIS
Stage 1
Cancer is small and is found in the breast tissue or in nearby lymph nodes
- Stage 1A = Primary tumour <2cm and has not spread outside of the breast
- Stage 1B = No tumour or primary tumour <2cm in the breast. There are a few cancer cells in nearby lymph nodes
Stage 2
Cancer is in the breast and has spread to nearby lymph nodes
- Stage 2A = No tumour in breast or primary tumour <2cm and cancer cells have spread to 1-3 of the nearby lymph nodes OR the primary tumour is 2-5cm but cancer cells have not spread to lymph nodes
- Stage 2B = Primary tumour 2-5cm and cancer cells have spread to the lymph nodes OR Primary tumour 2-5cm and cancer cells have spread to 1-3 of the nearby lymph nodes OR primary tumour >5cm and cancer cells have not spread to lymph nodes
Stage 3
Also known as locally advanced. Means the cancer has spread from the breast to nearby lymph nodes, the chest wall, or skin of the breast
- Stage 3A = No tumour or a primary tumour of any size within the breast tissue. Cancer cells are present in 4-9 of the nearby lymph nodes OR primary tumour is >5cm and cancer cells have spread to 1-3 of the nearby lymph nodes
- Stage 3B = Primary tumour of any size, cancer cells have spread to the chest wall and /or skin of the breast. May have spread to up to 9 nearby lymph nodes. Cancer that has spread to the skin may be inflammatory breast cancer.
- Stage 3C = No tumour or a primary tumour of any size within the breast tissue. Cancer may have grown into the chest wall or skin of the breast. Cancer cells have spread to lymph nodes: >10 in the armpit OR above/below the collarbone OR in the armpit and near the breast bone.
Stage 4
Also known as advanced, metastatic and secondary breast cancer. The cancer has spread beyond the breast or nearby lymph nodes to other parts of the body, such as the lungs or bones.
TNM staging
TNM staging is another way of describing the cancer’s size and spread. It uses tumour size (T), spread to nearby lymph nodes (N) and spread to other parts of the body (M) to give a detailed explanation of breast cancer. TNM staging can be pathological (pTNM) or clinical (cTNM):
- pTNM = when tissues from surgery are used for classification
- cTNM = when you care team classifies the cancer via tests and scans rather than surgery
Tumour (T): T1-T4, where a higher number suggests the tumour is larger. TX can be given is the tumour cannot be assessed and T0 can also be given when there is no evidence of a tumour.
Lymph Nodes (N): N1-N3, where a higher number suggests spread to more lymph nodes. NX is given when the lymph nodes cannot be assessed and N0 when no cancer cells are found in the lymph nodes.
Metastasis (M): MX if spread metastasis cannot be assessed, M0 if there are no signs of spread and M1 if there are signs of spread.
The combination of these categories gives the stage of the tumour. Cancer staging can vary, and be specific to each tumour and patient. Below is a common version of staging:
- Stage 0 – Carcinoma in situ. T0-1, N0, M0.
- Stage I – Localised cancer. T1-T2, N0, M0.
- Stage II – Local-advanced cancer in its early stages. T2-T4, N0, M0.
- Stage III – Local-advanced cancer in its late stages. T1-T4, N1-N3, M0.
- Stage IV – Metastatic advanced cancer. T1-T4, N1-N3, M1
What are the molecular subtypes of breast cancer?
Breast cancer can be divided into categories by testing to see if certain proteins are present on the cell surface or not. These categories are called molecular subtypes. Specific proteins can control how the cancer behaves and many breast cancer treatments have been made to target these proteins.
Hormone receptor status
Cancer cells with hormone receptors for the sex hormones oestrogen and/or progesterone on the surface are considered hormone receptor-positive (HR+). In HR+ breast cancers hormones can bind to these receptors on the cancer cell surface and affect how the cancer cells grow. This is the most common molecular subtype and accounts for up to 75% of breast cancers8,9,10.
Click to learn more about HR+ breast cancer.
HER2 status
Breast cancer cells can have high levels of the human epidermal growth factor (HER2) protein on the cell surface, meaning it is over expressed. This can lead to abnormal cell division and growth. These types of breast cancers are considered HER2-positive (HER2+) and account for around 20-25% of breast cancer cases11.
Click to learn more about HER2+ breast cancer.
Triple negative
When breast cancer cells lack hormone receptors and the HER2 protein on the cell surface they are considered triple negative. Triple negative breast cancer (TNBC) accounts for approximately 10-15% of breast cancers12,13.
Click to learn more about TNBC.
HER2-low
HER2-low is a new term used characterise breast cancer even further. It means that many breast cancer patients that were previously considered HER2-negative (HER2-) could now be considered HER2-low. This may provide a new treatment target for many secondary breast cancers. Evidence suggests up to 55% of all breast cancers may now be considered HER2-low14.
Find out more about HER2-low breast cancer here.
Did you know that the OWise app generates a personalised treatment report for you? After filling in details about your diagnosis a treatment report will be made that gives you easy to understand background information on your diagnosis and treatment possibilities. You can access this report with ease on-the-go.
Summary of receptor types:
- HR+: when a tumour is both PR+ and ER+
- HR-: when a tumour is both PR- and ER-
- ER+: oestrogen receptor is present
- ER-: oestrogen receptor is not present or active
- PR+: progesterone receptor is present
- PR-: progesterone receptor is not present or active
- HER2+: HER2 is present
- HER2-low: HER2 is present in low amounts
- HER2-: HER2 is not present or active
- TNBC: triple negative breast cancer, none of the above receptors are present or active
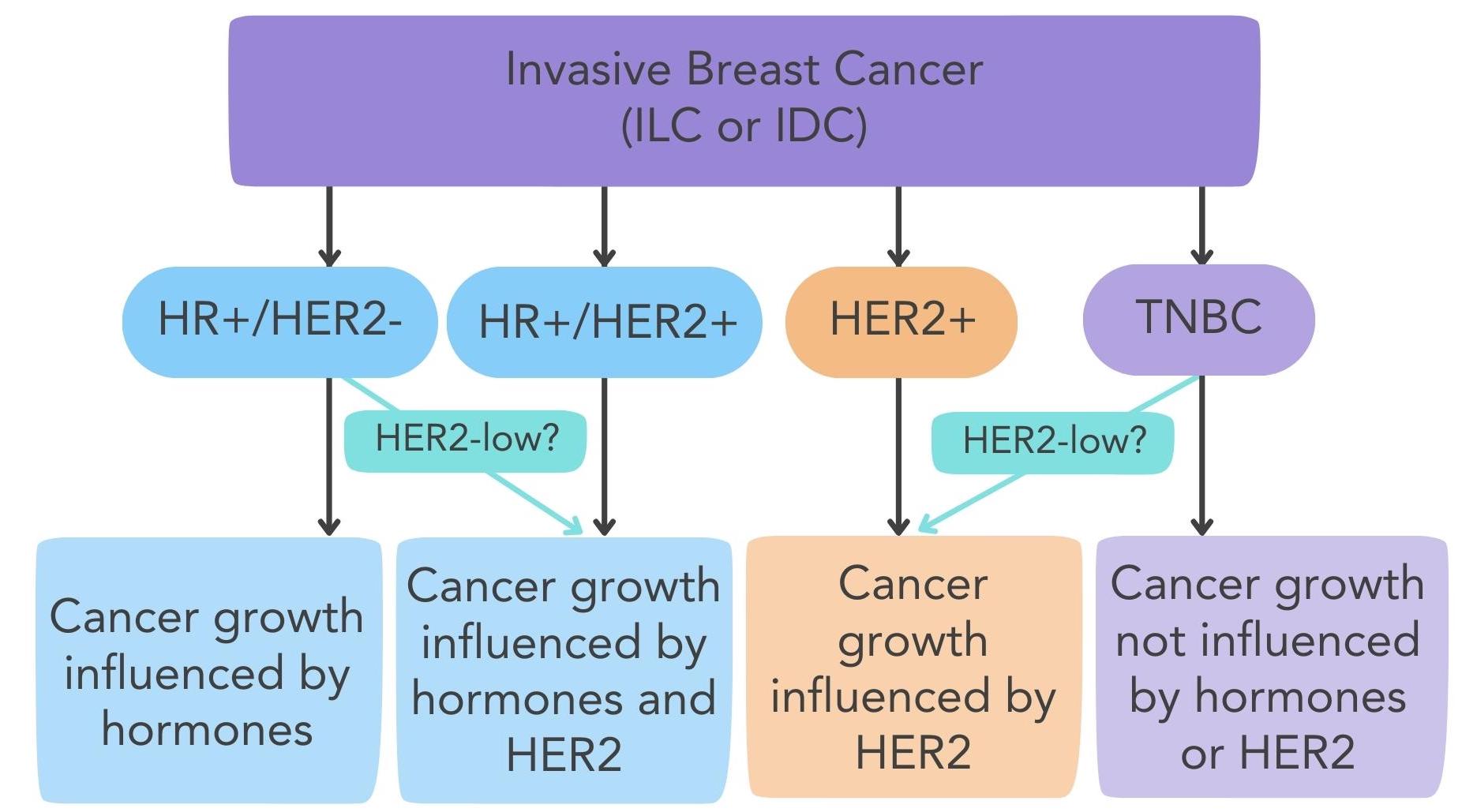
Figure 3. The different subtypes of invasive breast cancer
Tumour genomic tests
Tumour genomic tests may be done to measure the expression of certain genes in a piece of tissue from a tumour. The expression of these genes is seen as a measure of the activity of the gene. The level of activity of these can affect cancer behaviour, such as how likely it is to grow and spread. There are various tumour genomic tests available that can study tumour characteristics to see if certain treatments are needed or to estimate the risk of cancer returning. Usually, tumour genomic tests are recommended for people with early HR+ and HER2- breast cancer to determine if chemotherapy is needed as well as hormone therapy.
Genetic tests
A genetic test may be done if you have a significant family risk of breast/ovarian cancer or a genetic variant has been found in a family member15. Additionally, if you have been diagnosed with breast cancer before age 50, in both breasts, with TNBC or have Ashkenazi Jewish heritage. These tests can identify faulty versions of genes that can be passed down through families and can increase cancer risk, it is estimated that approximately 5-10% of breast cancers are caused by inheriting a faulty gene16. This includes genes such as the BRCA genes.
BRCA stands for breast cancer susceptibility gene and includes the BRCA1 and BRCA2 genes. Data suggests that having a faulty BRCA gene can increase the risk of someone developing breast cancer during their lifetime by 82%17. A genetic test to determine whether any genetic variants are present can help to inform treatment decisions, as there are now treatment options available to treat certain types of breast cancer in patients with a BRCA mutation.
To read more about the BRCA genes head over to the blog.
Understanding your pathology report
Everyone’s pathology report for diagnosis will be slightly different but will contain essential information about the characteristics of your breast cancer. It is a collection of lab reports prepared by pathologists telling you about which of the above categories your cancer fits into. This information is very valuable and determines what sort of treatment you may be given. For a more in-depth summary of what may be included in your breast cancer diagnosis pathology report and how to interpret it, see our ‘understanding your pathology report’ blog.
We hope this has helped you to understand your breast cancer diagnosis
As with every aspect of a breast cancer diagnosis, there will be things hard to understand, scary moments and a lot of information to process. It is really important to process your breast cancer diagnosis through trying to understand medical information and asking questions about anything you don’t understand.
At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Facebook for any updates. Any questions? Get in touch!
References
- World Health Organisation. Breast cancer. www.who.int. 2023 Jul 12. https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Overview
- Cancer Research UK. What is breast cancer? | Cancer Research UK. Cancerresearchuk.org. 2021 Jan 21. https://www.cancerresearchuk.org/about-cancer/breast-cancer/about
- National Cancer Institute. Breast Anatomy. training.seer.cancer.gov. https://training.seer.cancer.gov/breast/anatomy/
- American Cancer Society. Ductal Carcinoma in Situ (DCIS). www.cancer.org. 2021. https://www.cancer.org/cancer/types/breast-cancer/about/types-of-breast-cancer/dcis.html
- American Cancer Society. Invasive Breast Cancer (IDC/ILC). www.cancer.org. 2021. https://www.cancer.org/cancer/types/breast-cancer/about/types-of-breast-cancer/invasive-breast-cancer.html
- City of Hope. Breast Cancer Types. Cancer Treatment Centers of America. 2019 Jul 18. https://www.cancercenter.com/cancer-types/breast-cancer/types
- American Cancer Society. Treatment of Ductal Carcinoma in Situ (DCIS). www.cancer.org. 2021. https://www.cancer.org/cancer/types/breast-cancer/treatment/treatment-of-breast-cancer-by-stage/treatment-of-ductal-carcinoma-in-situ-dcis.html#:~:text=DCIS%20is%20considered%20non%2Dinvasive
- Nadji M, Gomez-Fernandez C, Ganjei-Azar P, Morales AR. Immunohistochemistry of estrogen and progesterone receptors reconsidered: experience with 5,993 breast cancers. American Journal of Clinical Pathology. 2005 [accessed 2022 Feb 20];123(1):21–27. https://pubmed.ncbi.nlm.nih.gov/15762276/. doi:https://doi.org/10.1309/4wv79n2ghj3x1841
- Lange CA, Yee D. Progesterone and Breast Cancer. Women’s Health. 2008;4(2):151–162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4038907/?report=classic. doi:https://doi.org/10.2217/17455057.4.2.151
- Moelans CB, de Ligt J, van der Groep P, Prins P, Besselink NJM, Hoogstraat M, ter Hoeve ND, Lacle MM, Kornegoor R, van der Pol CC, et al. The molecular genetic make-up of male breast cancer. Endocrine-Related Cancer. 2019 [accessed 2021 Dec 28];26(10):779–794. doi:https://doi.org/10.1530/erc-19-0278
- Arteaga CL, Sliwkowski MX, Osborne CK, Perez EA, Puglisi F, Gianni L. Treatment of HER2-positive breast cancer: current status and future perspectives. Nature Reviews Clinical Oncology. 2012;9(1):16–32. https://www.nature.com/articles/nrclinonc.2011.177/briefing/signup/?origin=Nature&originReferralPoint=EmailBanner. doi:https://doi.org/10.1038/nrclinonc.2011.177
- Lund MJ, Trivers KF, Porter PL, Coates RJ, Leyland-Jones B, Brawley OW, Flagg EW, O’Regan RM, Gabram SGA, Eley JW. Race and triple negative threats to breast cancer survival: a population-based study in Atlanta, GA. Breast Cancer Research and Treatment. 2008;113(2):357–370. doi:https://doi.org/10.1007/s10549-008-9926-3
- Plasilova ML, Hayse B, Killelea BK, Horowitz NR, Chagpar AB, Lannin DR. Features of triple-negative breast cancer: Analysis of 38,813 cases from the national cancer database. Medicine. 2016;95(35):e4614. https://pubmed.ncbi.nlm.nih.gov/27583878/. doi:https://doi.org/10.1097/MD.0000000000004614
- Li Y, Julia, Tam FY, Thomson Loong, Tse GM. Comprehensive characterization of HER2-low breast cancers: implications in prognosis and treatment. EBioMedicine. 2023;91(104571):104571–104571. doi:https://doi.org/10.1016/j.ebiom.2023.104571
- Lynch JA, Venne V, Berse B. Genetic Tests to Identify Risk for Breast Cancer. Seminars in Oncology Nursing. 2015;31(2):100–107. doi:https://doi.org/10.1016/j.soncn.2015.02.007
- CDC. Hereditary Breast Cancer and BRCA Genes | Bring Your Brave | CDC. www.cdc.gov. 2022 Sep 13. https://www.cdc.gov/cancer/breast/young_women/bringyourbrave/hereditary_breast_cancer/index.htm#:~:text=About%205%25%20to%2010%25%20of
- Shiovitz S, Korde LA. Genetics of Breast cancer: a Topic in Evolution. Annals of Oncology. 2015;26(7).
