
Urinary incontinence is a commonly experienced side effect of prostate cancer treatment. This is the first in a series of blogs where we will explore common side effects of prostate cancer and outline tips to help manage them. This blog will explore what urinary incontinence is, ways to manage this side effect, and how OWise can help you track it.
Incontinence can be experienced by up to 80% of men undergoing treatment.1 In the majority of men the incontinence is temporary, with 83% of men completely continent 24 months after surgery.2 The severity of incontinence and whether it goes away on its own depends on many factors such as your age and other health conditions.3 Regardless of how long incontinence lasts for you, it is a side effect that can greatly impact your quality of life. That’s why it’s important to know there are things you can do to improve and manage urinary incontinence.
What is Urinary Incontinence?
Urinary incontinence is the loss of the ability to control urination. This is a common outcome of certain treatments for prostate cancer such as radiation or surgery. There are a few specific types of incontinence:
- Stress incontinence often occurs during activities such as lifting something heavy or sneezing, and the pressure on your bladder causes some urinary leakage.3
- Urge incontinence refers to having the sudden strong urge to urinate and not being able to reach the bathroom in time.3
With OWise Prostate Cancer you can track problems with urination, number of incontinence pads used and degree of urinary pad saturation.
“Average saturation” was added as a tracker due to the variability between individuals in the frequency of when pads are changed. This is something that was stressed by the men that attended the OWise workshops.
How do these treatment options cause incontinence?
Usually, urine is stored in your bladder until it is full. Once it is full, the muscles of the bladder push and the urine flows from the bladder through a small tube called the urethra. In order to urinate, the muscles surrounding the urethra relax to allow the urine to pass through. These muscles surrounding your urethra (also known as urinary sphincter) and pelvic floor muscles are very important in controlling urinary flow.4 These muscles, certain nerves, the bladder and the urethra all work in coordination to release urine on command.
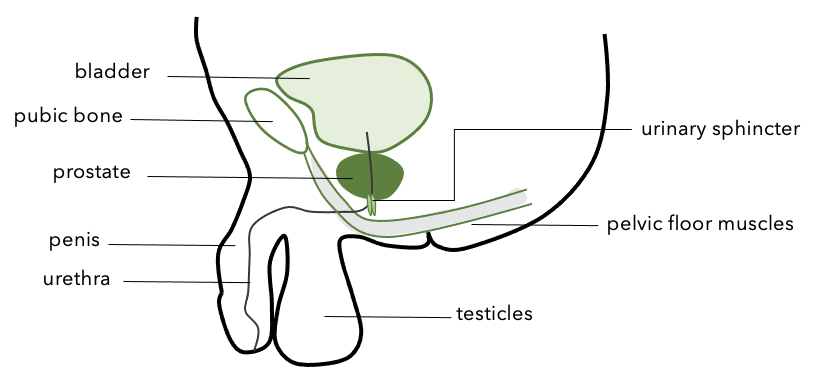
Figure 1: Outline of pelvic floor muscles and urinary sphincter in relation to the prostate and bladder. Figure adapted from Prostate Cancer UK and Memorial Sloan Kettering Cancer Center.
Since the prostate gland sits directly underneath your bladder and very close to the muscles surrounding your urethra, both surgery and radiation to this area can affect and damage these nerves and muscles, as well as your pelvic floor muscles.
What are known tips to help manage incontinence?
We have compiled a list of some helpful exercises, resources and other interventions that may help you manage urinary incontinence.
“It’s hard to believe, but urinary control does continue to improve over two years, and occasionally, even longer than that. For many men, the recovery of urinary control is a slow process. The most important thing you can do is not get discouraged.” – JP Mac, writer and prostate cancer patient
- Exercises: exercises that strengthen your pelvic floor muscles, such as kegel exercises, can help control your urine flow because these muscles help control your urinary flow. These exercises should be done both before and after surgery. If you’d like more details on how to correctly perform these exercises check out these resources:
- Resources: There are plenty of resources to help manage incontinence in your day to day life. Here are a few that may help:5
- Urinary pads & absorbent pants: you may be able to obtain these for free from local NHS services
- For increased access to public toilets, the National Key Scheme created by Disability Rights UK grants you access to locked public toilets around the country and Prostate Cancer UK’s Urgent Toilet Card can help you to ask when you need faster access to a toilet.
- Handheld Urinals
- Absorbent bed lining
- Urinary sheath: these fit around your penis and drain into a bag which can be concealed inside your trousers or clothes. Check out this article for more information on how to use and choose a urinary sheath.
- Biofeedback therapy: this is a non-invasive method to help with bladder control. It occurs over several sessions and involves using electrodes to visualise muscle contractions.6 The aim is to help make you more conscious of these muscles and how to control them.
- Planning and dietary changes: You may have to plan your outings more carefully and ensure that you’ll be able to stop and access a toilet when needed. Reducing your intake of fluids, and especially of alcoholic and caffeinated drinks can also help lessen the need to urinate.
- Are there medical interventions that can help? If you are still suffering from incontinence one year after treatment, there are medical interventions that may be available for you. These include medications that decrease frequency of urination, an artificial urinary sphincter and an internal male sling. Discuss these options with your care team if you are still experiencing incontinence 6 to 12 months after treatment.5
Incontinence is an issue that affects many men after treatment for prostate cancer and that often can and does improve with time and intervention. Given how common urinary incontinence is, there should be no stigma or shame in speaking openly about it.
These are a few resources if you would like to read more about other people’s experience of incontinence after prostate cancer treatment:
- JP Mac is a writer who underwent surgery for prostate cancer who wrote about his experience in a short e-book called “They Took my Prostate: Cancer, Loss and Hope”. For information about the author, and his specific struggle with incontinence check out this article.
- There are many online patient forums which discuss incontinence and prostate cancer; these may help to get a sense of common issues and how people deal with them.
How can OWise help?
OWise Prostate cancer is an app that aims to support and help men regain control throughout diagnosis and treatment of prostate cancer. The app was co-designed with prostate cancer patients in workshops held across the UK to ensure that the app is useful for those with prostate cancer. Because of this, it has specific features to monitor prostate cancer post-treatment urinary incontinence. The feedback that we received highlighted that this side effect would be useful to monitor and track.
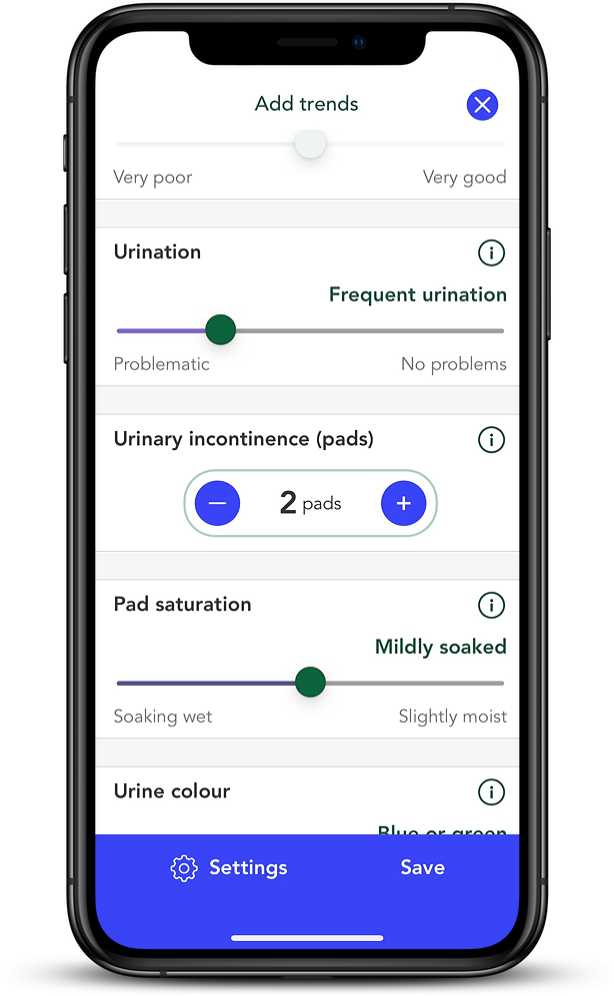
OWise has over 30 different trackers which allow you to input your daily experience of various side effects. These are the specific trackers designed to address incontinence:
- Frequency of or problems with urination
- Number of urinary incontinence pads used
- Degree of urinary pad saturation (Average saturation)
Tracking these and other side effects will allow you to view any changes or progressions in your own graph which can be shared with your care team. This could be helpful to assess whether management techniques you are trying are working and, if so, which one is most effective. It may also be helpful to see how incontinence progresses (and perhaps improves) naturally over time. Having an accurate and detailed record of any changes to the severity of incontinence can improve and facilitate communication with your care team.
To learn more about OWise app trends and how to get the
most out of this feature head to our tracking side effects blog.
We hope this blog has given you a useful overview of urinary incontinence, signposted helpful resources and management tips to address this incontinence. Remember not to suffer in silence, your care team will have experience treating incontinence.
References
- Hoyland, Kimberley et al. “Post-radical prostatectomy incontinence: etiology and prevention.” Reviews in urology vol. 16,4 (2014): 181-8.
- Sacco, Emilio et al. “Urinary incontinence after radical prostatectomy: incidence by definition, risk factors and temporal trend in a large series with a long-term follow-up.” BJU international vol. 97,6 (2006): 1234-41. doi:10.1111/j.1464-410X.2006.06185.
- Grise, Philippe, and Scott Thurman. “Urinary Incontinence Following Treatment of Localized Prostate Cancer.” Cancer Control, vol. 8, no. 6, 2001, pp. 532–539., doi:10.1177/107327480100800608.
- “Urinary Incontinence in Men.” Urinary Incontinence in Men | Michigan Medicine, www.uofmhealth.org/health-library/zp1188#zp1191.
- “Urinary Problems after Prostate Cancer Treatment.” Prostate Cancer UK, prostatecanceruk.org/prostate-information/living-with-prostate-cancer/urinary-problems.
