Joint pain is one of the most common symptoms for those taking Aromatase Inhibitors (AIs), such as anastrozole, as their form of hormone treatment. Whilst for some this can lead to mild or moderate symptoms, for others the severity can make it difficult to complete simple daily tasks, carry out their vocation or even spend time with their families. However, research has shown us that there are a number of effective options for those experiencing these symptoms to manage their symptoms and alleviate their pain, resulting in a less disruptive treatment.
Because AIs can prevent breast cancer recurrence, minimising the common side-effect of joint pain is crucial to getting the benefit of long-term use. In this blog, we will discuss the various ways of coping with this and look at some practical solutions for those who find themselves experiencing this common symptom. We will also discuss what to do in the event that simply managing the pain is not feasible, and a different approach becomes necessary.
What are Aromatase Inhibitors (AIs)?
Aromatase inhibitors are a treatment prescribed to hormone receptor positive breast cancer patients. Hormone receptor positive means that the cancer cells grow in response to the hormones oestrogen and/or progesterone (for more information about this, check out our Pathology blog). Aromatase inhibitors are usually given as an adjuvant therapy (after surgery) to postmenopausal women to help reduce the risk of breast cancer returning. This medication comes in pill form and is usually taken once a day for a period of around 5 to 10 years.
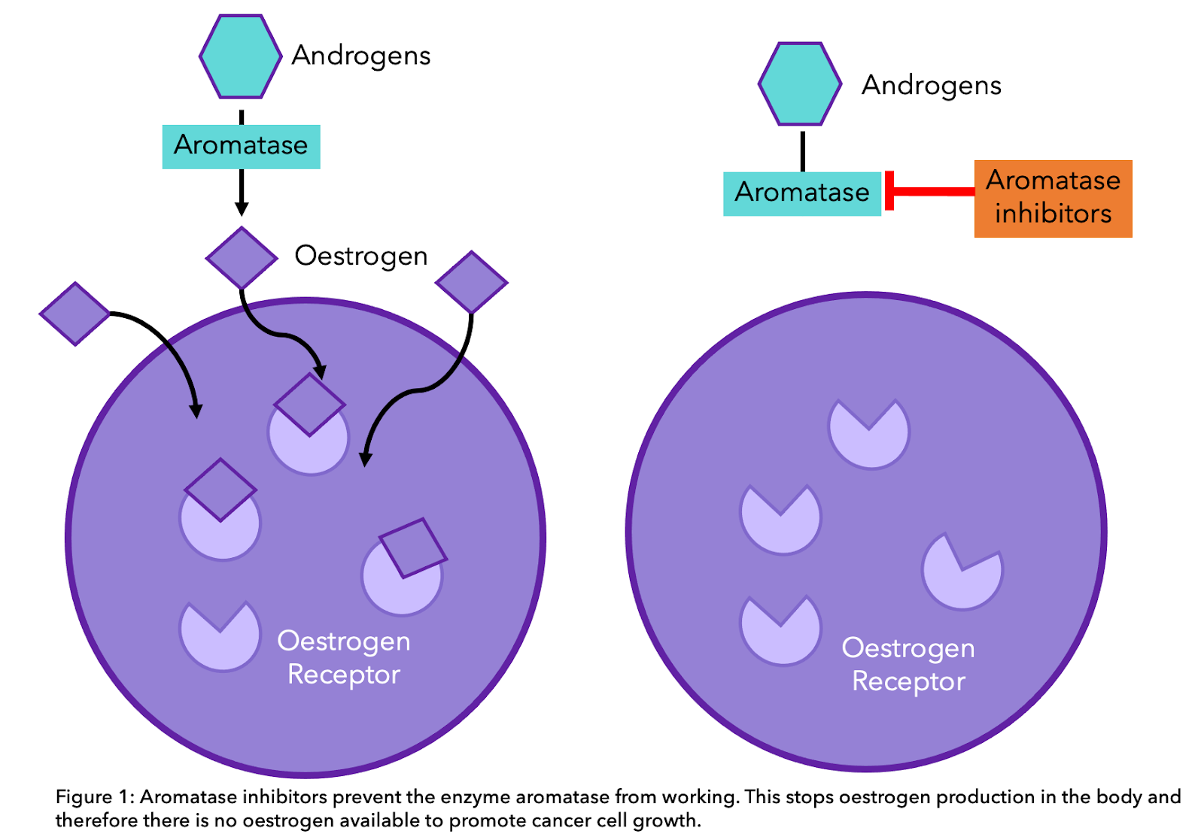
For premenopausal women, the main source of oestrogen and progesterone are the ovaries. In postmenopausal women, once the menstrual cycle has ceased, the main source of oestrogen is from the aromatase pathway. This is where androgens (sex hormones like testosterone) created in the adrenal glands and ovaries are converted to oestrogen. This happens all over the body, including in the liver, muscle but most significantly in the fat under the skin. Aromatase inhibitors work by preventing the enzyme “aromatase” from converting these hormones into oestrogen, thus oestrogen production is stopped. This way, AIs effectively help to stop any remaining cancer cells from growing (see diagram below) [1]. For more information about hormone receptor positive breast cancer, check out these previous blogs on the early and late stages as well about the key differences between aromatase inhibitors and tamoxifen.
The three main kinds of AI are:
-
Arimidex® (anastrozole)
-
Femara® (letrozole)
-
Aromasin® (exemestane)
Anastrozole, letrozole and exemestane are third generation AIs, and often decrease circulating oestrogen to undetectable levels, thereby reducing tumour proliferation and growth [2]. Moreover, AI therapy has been demonstrated to reduce the rate of mortality in breast cancer by up to 40% [3]. However, as we will see in the next section, joint pain is one of the most common side effects.
The Biology of Joint Pain
Joint pain, or arthralgia, appears to be a relatively common side effect. In a review including 13,177 patients, 20-70% of participants experienced this side effect [4]. Joint pain caused by aromatase inhibitors can be experienced in a variety of locations but most commonly in the fingers, wrists, shoulders, knees and ankles [5]. Joint pain can begin at approximately 2 months after the start of treatment and to peak at around the 6-month mark, but it can appear up to 2 years after initiation of therapy [6].
The suggested cause of joint pain is the drop in circulating oestrogens by aromatase inhibition in postmenopausal women. This hypothesis is supported by the observation that backaches, joint pains, and stiffness are commonly experienced among perimenopause (or menopause transition) and postmenopausal women in the general population. Although oestrogen has no specific effect on the joint structures that could cause pain, it can influence inflammation and the nervous pathway that connects the brain with the rest of the body to enable the feeling of pain [7].
When it comes to determining the severity of the pain in the joints, a comparative 5 year trial (ATAC) was conducted. The aromatase inhibitor anastrozole was compared to another hormone therapy, Tamoxifen. They found that joint pain and bone fractures were more common in those taking AIs [6]. However, the same trial also noted that intensity of joint pain did not often reach severe levels:
In most patients the events (of joint pain symptoms) were mild-to-moderate in intensity and did not lead to withdrawal of treatment.
Budzar et al., 2006 (speaking about the ATAC Trial) [6]
There hasn’t been enough evidence to find consistent variables that can predict the incidence of AI-induced joint pain. However, some studies point to previous treatments as predictors for the increased likelihood of this symptom. For example, a recent study found that patients previously treated with tamoxifen experienced greater pain when they switched to AIs and had an excess risk of stopping the therapy the first 12 months [8].
Methods for Managing Joint Pain
Before exploring these methods, remember that if you are experiencing joint pain due to your hormone therapy, or for any other breast cancer related cause, using the OWise breast cancer app you can track how this changes over time. Using the trends feature, you can input the severity of your pain as it changes throughout the week, month or year and review this at any time. Try incorporating the following suggestions into your routine and see for yourself how your pain levels change.
Incorporating Exercise
When you are experiencing joint pain, it might seem that exercise will just make things worse, but, in fact, avoiding exercise will inevitably lead to joint pain continuing and worsening over time. This is because with regular exercise, the muscles around the joints gain strength and flexibility, offering a layer of protection against pain and injury. While pain medication and some complementary therapies can be incredibly effective at providing short term relief, recent studies have demonstrated that exercise can relieve musculoskeletal symptoms and improve quality of life in the long run [9]. A particular study conducted with 121 postmenopausal women found that their average pain and worst pain scores dropped by around 20% after moderate regular exercise [10]. One of the researchers in this study, Dr. Melinda Irwin, said:
“In this study, we discovered that exercise improves joint pain, the most common side effect of aromatase inhibitor use.”
Dr. Melinda Irwin, Associate Cancer Center Director at Yale University [10]
So what kinds of exercises are the most effective? Here are a few variations that can help specifically with joint pain:
- Going for a walk
Going for a regular walk can help put some gentle pressure on your knee and ankle joints and build up some strength. It can also help with weight loss which can reduce the constant pressure on your joints when you’re standing up or walking around.
- Weight-bearing Exercises
The same study mentioned by Dr Irwin above, known as the HOPE study (Hormones and Physical Exercise) [10], found that more intense strength based training helped to reduce the eventual pain scores even further. There are many resources where these types of exercises can be found, please have a look at this BreastCancer.org page.
- Yoga and Pilates
Flexibility is also key to manage joint pain, and can prevent the stiffness that is also associated with using AIs. Yoga and pilates can both help with accessing the full range of motion, helping you to avoid stiff and inflexible muscles and protect against pain [11].
The amount of exercise you do also makes a difference. You may find that since the active treatment period, your capacity for exercise is not the same as it used to be and your limits have changed somewhat. This is very natural, and finding what level of exercise is comfortable and reasonable for you is part of that adjustment process.
But remember, while it can be good to push beyond those limits, it’s more important to find a new normal which is sustainable for regular exercise. Even if your walks are not as long or your sessions are not as intense, exercising moderately and consistently will support your joints in the long run and prevent unnecessary injuries.
It can even be a good idea to start these kinds of exercises prior to experiencing joint pain or even prior to taking the medication. That way, the protection that it can offer will already be in place before any symptoms begin to show. Equally, because of the stress and strain that the joints are under during the treatment, the symptoms of pain and stiffness do not always subside once the treatment is over. Therefore, making this a part of your routine will be more effective the earlier you do it.
Adjustments to Diet
Slight adjustments to your diet can help with managing joint pain when using Aromatase Inhibitors. Here are a few suggestions that can have a long-term benefit:
- Weight Loss
The first consideration follows on from the last, and can be achieved either through increased exercise, a change to your diet or a combination of the two. Especially if your pain is localised around your knee or ankles, excess weight can exert pressure on your joints and weaken them over time. Planning regular meals, drinking plenty of water and reducing portion size can all help with weight loss, as well as reducing the amount of fat and sugar in the foods in your diet [12].
- Calcium and Vitamin D
While calcium is essential for building strong bones, vitamin D is also very important. This is because vitamin D helps the body to absorb calcium, and so make sure you don’t include one in your diet without the other. Severe hypovitaminosis D has been reported to be prevalent in patients with persistent musculoskeletal pain and has been postulated as a potential cause of pain in women on aromatase inhibitors [13].
The sources of calcium include yoghurt, cheese and other dairy products, leafy vegetables like spinach or kale, fish such as sardines or salmon and some nuts and beans. Vitamin D can be included in your diet by eating more oily fish like mackerel or herring, red meat, liver, egg yolks and cereals. This can also be gained by taking vitamin D supplements. Because we can produce our own vitamin D using sunlight, it’s even more important to have a source of dietary vitamin D during the winter months [14].
Adding or Switching Medication
If your symptoms are temporary and not too intense, then you could consider using these pain relief medications. When it comes to anti-inflammatory drugs, make sure to discuss the type and dosage with your doctor first in case it might conflict with your existing medication and cause further problems.
- Paracetamol
- NSAIDs (e.g ibuprofen)
- Opioid Analgesics (e.g morphine)
According to the ATAC trial, 90% of those who did experience AI-induced joint pain were able to manage their symptoms using just one NSAID or a mild analgesic [6]. However, as we mentioned before, it can be the case that pain is more intense and continues for an extended period of time. In this instance, it is worth discussing alternative measures with your doctor.
As described above, there are three different aromatase inhibitors, and while they all serve the same purpose in helping to reduce the recurrence of cancer, they are slightly different and affect patients in different ways. Because of this, simply switching from one AI to another can be a potent remedy to the issue of joint pain.
“In patients intolerant to one AI, switching to another [aromatase inhibitor] allows a higher proportion of patients to continue the therapy and maximize hormonal adjuvant therapy and disease outcome benefits.”
Briot et al., 2010 [15]
Make sure to keep your doctor up to date about how your joint pain is changing. This means that if the pain does become very severe, they will have time to consider which other AI to provide you with and create a new treatment plan for you. It also means that there will be less time in between medications, resulting in a shorter interruption period and a continued low chance of cancer recurrence.
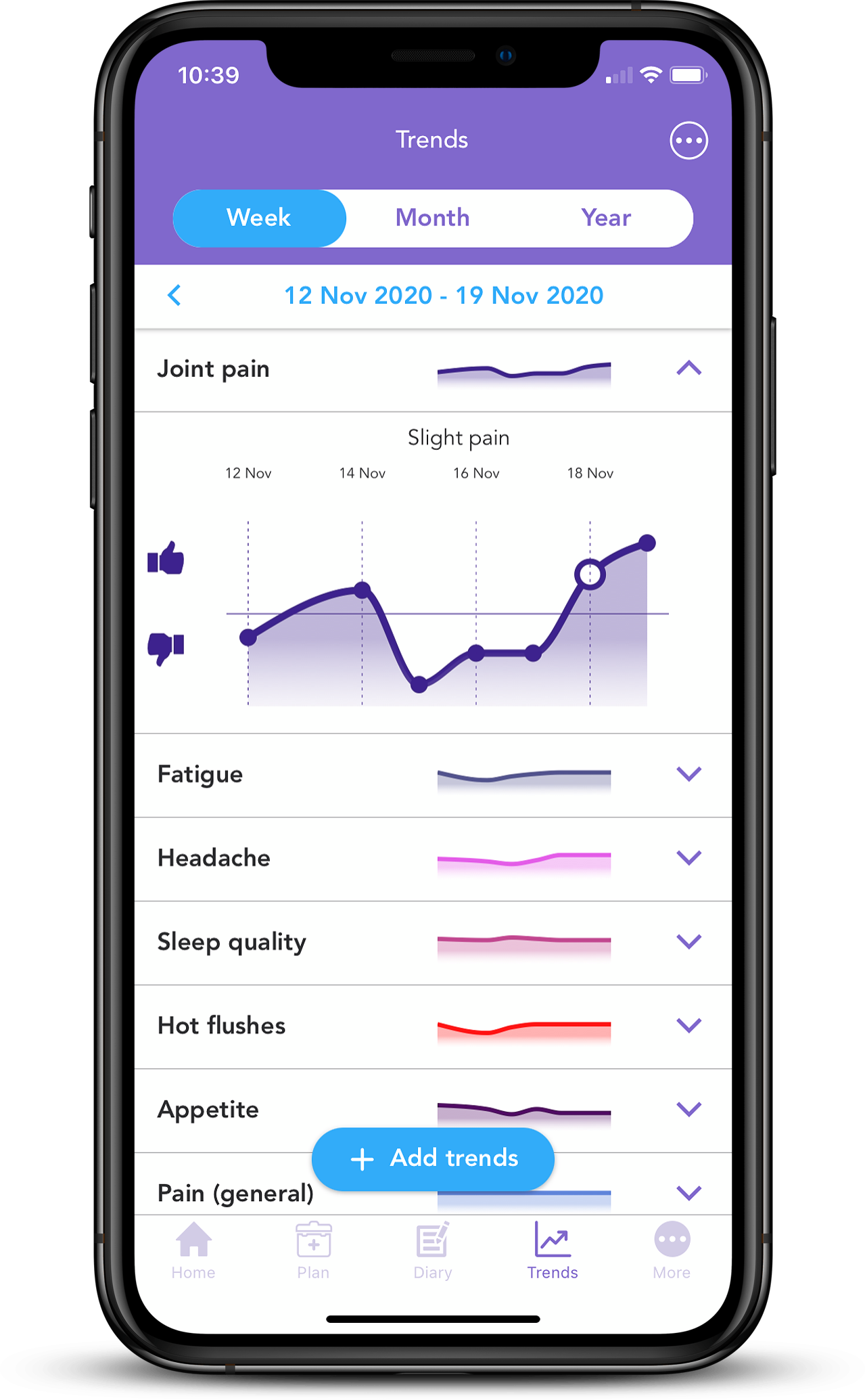
As we mentioned before, keeping track of your symptoms as they change is easier than ever with the OWise breast cancer app. Using the trends feature you can visualise how your symptoms change over time. Having more information at your fingertips can help improve communication with your care team and make sure you receive the best care possible. Download the free app today.
Useful Links
Breastcancer.org: Aromatase Inhibitors
Breastcancer.org: Bone and Joint Pain
Cancer.org: What are the Risks and Side Effects of Aromatase Inhibitors?
Breast Cancer Now: 5 Commonly Asked Questions about Hormone Therapy Joint Pain
References
[1] Francis, P.A., Regan, M.M., Fleming, G.F., Láng, I., Ciruelos, E., Bellet, M., Bonnefoi, H.R., Climent, M.A., Da Prada, G.A., Burstein, H.J. and Martino, S., 2015. Adjuvant ovarian suppression in premenopausal breast cancer. New England Journal of Medicine, 372(5), pp.436-446.
[2] Geisler, J., Haynes, B., Anker, G., Dowsett, M. and Lønning, P.E., 2002. Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. Journal of Clinical Oncology, 20(3), pp.751-757.
[3] Freedman, O.C., Fletcher, G.G., Gandhi, S., Mates, M., Dent, S.F., Trudeau, M.E. and Eisen, A., 2015. Adjuvant endocrine therapy for early breast cancer: a systematic review of the evidence for the 2014 Cancer Care Ontario systemic therapy guideline. Current oncology, 22(Suppl 1), p.S95.
[4] Beckwée, D., Leysen, L., Meuwis, K. and Adriaenssens, N., 2017. Prevalence of aromatase inhibitor-induced arthralgia in breast cancer: a systematic review and meta-analysis. Supportive Care in Cancer, 25(5), pp.1673-1686.
[5] Younus, J. and Kligman, L., 2010. Management of aromatase inhibitor–induced arthralgia. Current Oncology, 17(1), p.87.
[6] Buzdar, A.U., 2006. Clinical features of joint symptoms observed in the ‘Arimidex’, Tamoxifen, Alone or in Combination (ATAC) trial. Journal of Clinical Oncology, 24(18_suppl), pp.551-551.
[7] Felson, D.T. and Cummings, S.R., 2005. Aromatase inhibitors and the syndrome of arthralgias with estrogen deprivation. Arthritis & Rheumatism, 52(9), pp.2594-2598.
[8] Pineda-Moncusí, M., Servitja, S., Tusquets, I., Diez-Perez, A., Rial, A., Cos, M.L., Campodarve, I., Rodriguez-Morera, J., Garcia-Giralt, N. and Nogués, X., 2019. Assessment of early therapy discontinuation and health-related quality of life in breast cancer patients treated with aromatase inhibitors: B-ABLE cohort study. Breast cancer research and treatment, 177(1), pp.53-60.
[9] Lu, G., Zheng, J. and Zhang, L., 2020. The effect of exercise on aromatase inhibitor-induced musculoskeletal symptoms in breast cancer survivors: a systematic review and meta-analysis. Supportive Care in Cancer, 28(4), pp.1587-1596.
[10] Arem, H., Sorkin, M., Cartmel, B., Fiellin, M., Capozza, S., Harrigan, M., Ercolano, E., Zhou, Y., Sanft, T., Gross, C. and Schmitz, K., 2016. Exercise adherence in a randomized trial of exercise on aromatase inhibitor arthralgias in breast cancer survivors: the Hormones and Physical Exercise (HOPE) study. Journal of Cancer Survivorship, 10(4), pp.654-662.
[11] Perfectly Pilates. 2017. Soothe Painful joints with pilates. [online]. Available at: https://perfectlypilates.co.uk/soothe-painful-joints-with-pilates/
[12] NHS. 2019. 12 tips to help you lose weight. [online]. Available at: https://www.nhs.uk/live-well/healthy-weight/12-tips-to-help-you-lose-weight/
[13] Taylor, M., Rastelli, A., Civitelli, R. and Ellis, M., 2004. Incidence of 25-OH vitamin D deficiency in patients with a history of breast cancer who have musculoskeletal symptomatology. Breast Cancer Research and Treatment, 88.
[14] NHS. 2020. Vitamins and Minerals. [online]. Available at: https://www.nhs.uk/conditions/vitamins-and-minerals/
[15] Briot, K., Tubiana-Hulin, M., Bastit, L., Kloos, I. and Roux, C., 2010. Effect of a switch of aromatase inhibitors on musculoskeletal symptoms in postmenopausal women with hormone-receptor-positive breast cancer: the ATOLL (articular tolerance of letrozole) study. Breast cancer research and treatment, 120(1), pp.127-134.