In the first of our series ‘Breast cancer under the microscope’ we have focused on the pathology results. You should be given these each time a tissue is removed, either from a biopsy, breast-conserving surgery or mastectomy. They contain a lot of information and it can be difficult to process it all. That’s why we have created a comprehensive resource that can be used as a reference to help you better understand the information you have been given.
Your pathology results contain valuable information that will determine the type of treatment you receive. They are not always given to you by your clinical team, however, it is important to ask your doctor or nurse for a copy. This can help you better understand your diagnosis and treatment plan. This knowledge is key for you to be able to meaningfully participate in conversations with your clinical team, make informed decisions and ask the right questions. Start learning all the nitty-gritty details of a pathology report!
Did you know that OWise breast cancer app generates suggested questions for each user based on their breast cancer type? When you enter your cancer profile details (tumour size, hormone receptor status, HER2 status, BRCA1/2…) the smart software of OWise creates list of questions that are specifically relevant for you, to help guide conversations with your care team.
What is pathology?
Pathology is the science that studies the cause and effect of diseases, and to do so pathologists examine samples of body tissues, in our case of breast cancer. Specifically, pathologists stain tissue slices from your breast cancer sample with different markers that they then analyse under the microscope (the diagram below is an example of what they look like). After extensive examination, the pathologist writes a report about your cancer sample.
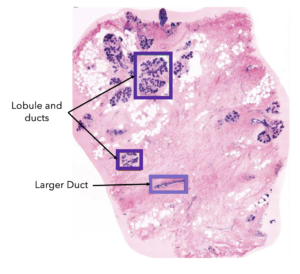
An example of breast tissue under a microscope1.
The sample that the pathologist receives can be tissue from a biopsy (tissue sample), breast-conserving surgery (removal of cancer and a small section of normal breast tissue surrounding it), or a mastectomy (removal of all breast tissue including the nipple area). The amount of detail in each report will depend on what tissue you’ve had removed and how much.
Not all reports will include the same amount of information. For example, a pathology report of a biopsy will have significantly less detail than a report following surgery. There is also variation between hospitals in the layout and terms used. This blog provides a guideline of the most commonly included aspects of a pathology report but takes note that it may not look identical to yours.
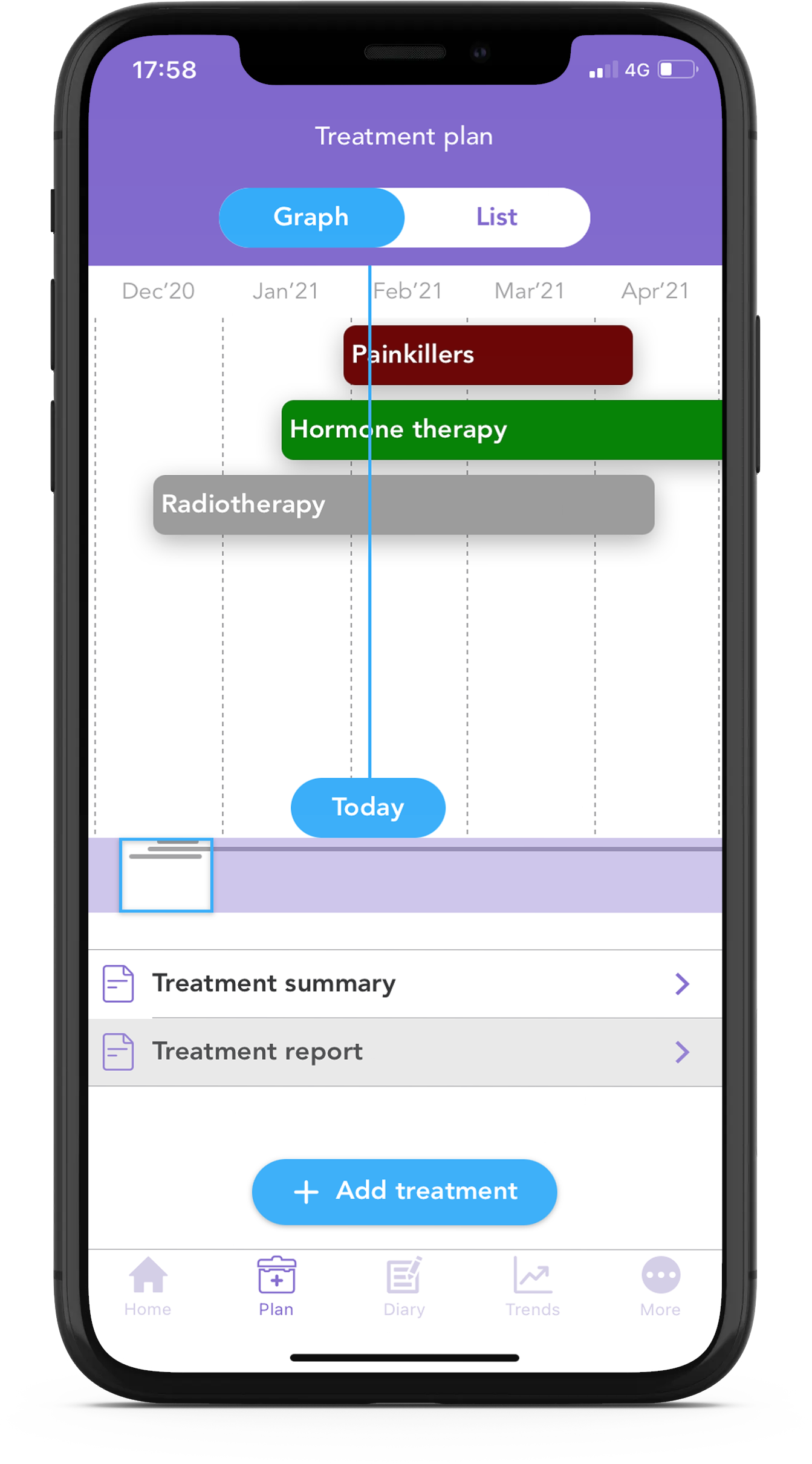
Want to keep track of all the information from your treatment report? With the OWise breast cancer app you can input your details about your treatment and review the information at any time. Stay informed with OWise!
Helping you to better understand your pathology results
What is my breast cancer type?
“Invasive” versus “In Situ”
If the report specifies that the cancer is Invasive, it means that the cancerous cells have grown past the part of the breast location where they originated from. However, if the report specified the cancer as In Situ (“In the original place” in Latin”), it means that the cancerous cells have not grown past the breast tissue location where they originated from.
“Ductal” versus “Lobular”
The female breast is made up of 12–20 sections called lobes. Each of these lobes is made up of many smaller lobules, the gland that produces milk in nursing women. Both the lobes and lobules are connected by milk ducts, which act as stems or tubes to carry the milk to the nipple (see picture below).
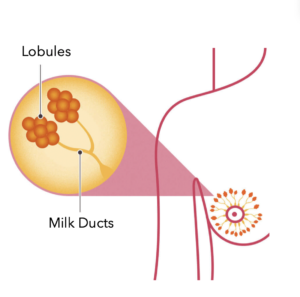
Diagram showing lobules and milk ducts2.
The report will explain what type of cells are cancerous. If the cancer cells originated at the ducts where the milk travels to the nipple, the cancer is Ductal, while if it originated at the milk-producing lobules, the cancer is Lobular.
With these simple definitions, you can easily understand your type of cancer:
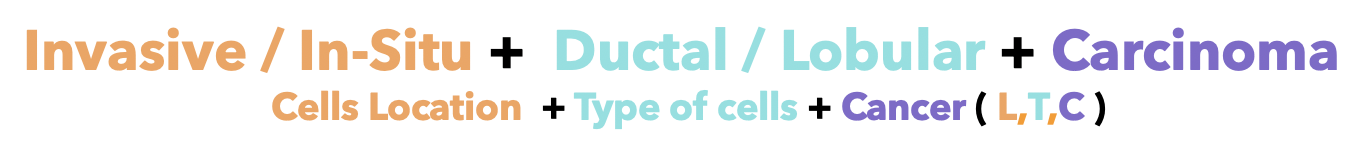
There are around 55,200 new breast cancer cases in the UK every year, that’s around 150 every day (2015-2017)3. The most common type of cancer is Invasive Ductal Carcinoma (IDC) with approximately 70% of all the new breast cancer diagnosis. Approximately 20% corresponds to Ductal Carcinoma in Situ 4 and 10-15% to Invasive Lobular Carcinoma. There are other less common breast cancers5 such as Inflammatory, Paget’s, papillary or mucinous among others (Lobular Carcinoma in Situ is not classified as cancer).
Does the size of the cancer matter?
The report will also specify the size of the cancerous cells (tumour). The size is measured at cancer’s widest point and is usually described in millimetres (mm). In the case of finding two tumours together, one Invasive and another In Situ, the combined size will be measured as the whole tumour size. However, only the invasive breast cancer will be further examined by your care team. In case you have a tumour larger than 3 cm (30 mm), you might receive treatment like chemotherapy before surgery to reduce the size. Treatment before surgery is technically referred to as neoadjuvant 6.
Although smaller breast cancers often have better outcomes, other factors including the rate of growth of the cells also need to be taken into consideration.
What is the Grade of my cancer?
Pathologists classify cancer cells in different grades depending on how different they look to normal breast cells and how quickly they are growing. The grades range from 1-3, with 1 being physically closest to normal breast cancer cells and 3 being the most abnormal. This is not the same as the stages of breast cancer, which is not in your pathology report. To learn more about stages, head to the bottom of this blog or to our Instagram post.
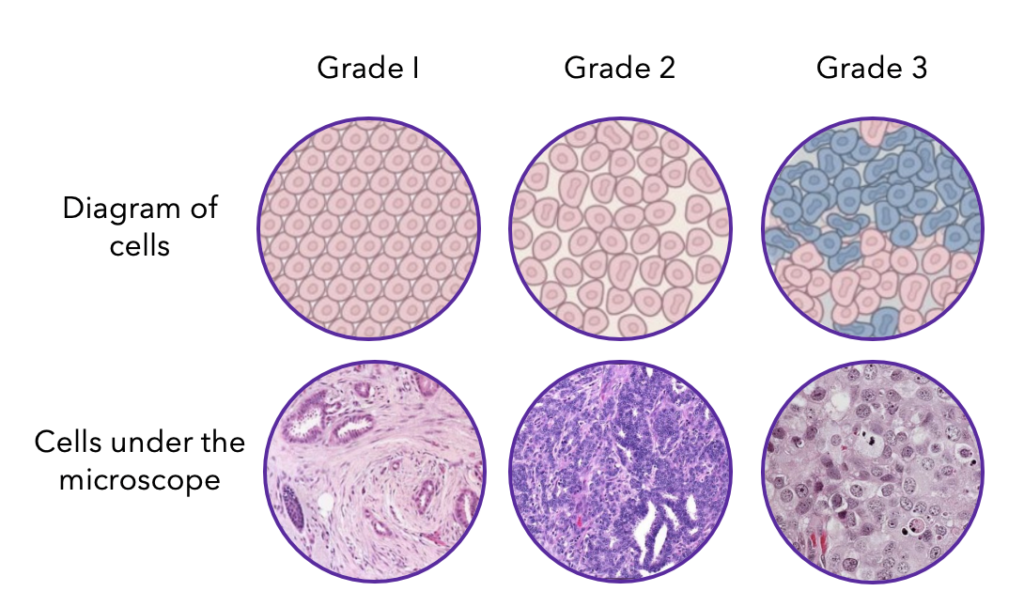
Grades of breast cancer7.
Why did they test for hormone receptors?
Some breast cancer cells grow in response to the hormones oestrogen and progesterone. If your pathology report specifies that you are positive to the oestrogen and/or progesterone receptors (ER+ and/or PR+), it means that your breast cancer cells grow and divide in response to these hormones. Furthermore, it means that you may benefit from hormonal therapy that blocks the effects of these hormones.
Your pathology report will likely give a score indicating the amount of hormone receptors per cancer cell and the proportion of cells with receptors. You’ll likely see a score between 0 and 8, with a higher score signifying the more ER+ the breast cancer is. The proportion of cells with receptors can also be given in a percentage from 0% to 100%. where more than 1% is characterised as ER+8.
What is HER2?
HER2 is a protein that helps control how cells grow, divide and repair themselves. Cancer cells with too many copies of the HER2 protein on their surface tend to grow particularly fast.
Multiple tests can be done to test the presence of HER2 on cell surfaces. If tested positive, HER2-specific treatments can be included in your treatment plan. A common treatment is Herceptin, which you can find out more about in our HER2 blog.
What is HER2-low?
Until recently, breast cancer was either considered HER2-positive or HER2-negative. Now, it is possible to characterise breast cancer as HER2-low. Research suggests up to 55% of breast cancer cases are now considered HER2-low9.
If you were previously classified as HER2-negative, it is possible that you could now fall into the HER2-low category. This provides a new treatment target for many secondary (metastatic, advanced) breast cancers. There is currently an approved treatment option for HER2-low secondary breast cancer in the US and Europe10,11.
For more on how HER2-low breast cancer is measured, how common it is, and treatment options, check out the blog ‘What is HER2-low Breast Cancer?’.
What is lympho-vascular invasion?
In the breast, there is a network of blood and lymphatic vessels which connect the breast tissue to the rest of the body. The lymphatic vessels are part of the lymphatic system, which is a network of tissues and organs (lymph nodes) that help get rid of the body of toxins, waste and unwanted materials. If your report mentions lympho-vascular invasion, it means that the cancer cells have reached these vessels and have a higher chance of spreading to other parts of the body.
Has the breast cancer cells spread to the lymph nodes?
Breast cancer cells often first spread to the lymph nodes under your arm (axillary lymph nodes). Normally either before or after your surgery, a few lymph nodes are removed to check for any breast cancer cells. This can be completed through a Sentinel lymph node biopsy and the results will show whether the lymph nodes are positive (contain breast cancer cells) or are negative (breast cancer-free).
Genomic profiling?
Genomic tests identify a set of genes that can affect how a cancer is likely to behave and respond to treatment. These tests are usually only carried out in breast cancers that are invasive, ER+, HER2 negative and with no more than three lymph nodes containing cancer cells. This is because in these cases it is not clear whether the type would benefit from chemotherapy, which can be indicated through the results of these tests. There is a variety of tests available, including Oncotype DX and Endopredict, that will be discussed in detail as part of this series of blogs.
Familial breast cancer and BRCA risk testing
A family history of cancer can increase the risk of developing breast cancer. One of the most well-known genes responsible for this is BRCA. If you have a family history of breast cancer, you can be offered a BRCA genetic test through the NHS. To find out more about BRCA, head to our BRCA blog.
What does my Ki67 score signify?
Ki67 is a protein found in cells that shows how quickly cells are dividing and growing. In breast cancer, it is considered a high score if Ki67 is expressed in more than 20% of the cells analysed.
Has breast cancer been completely removed?
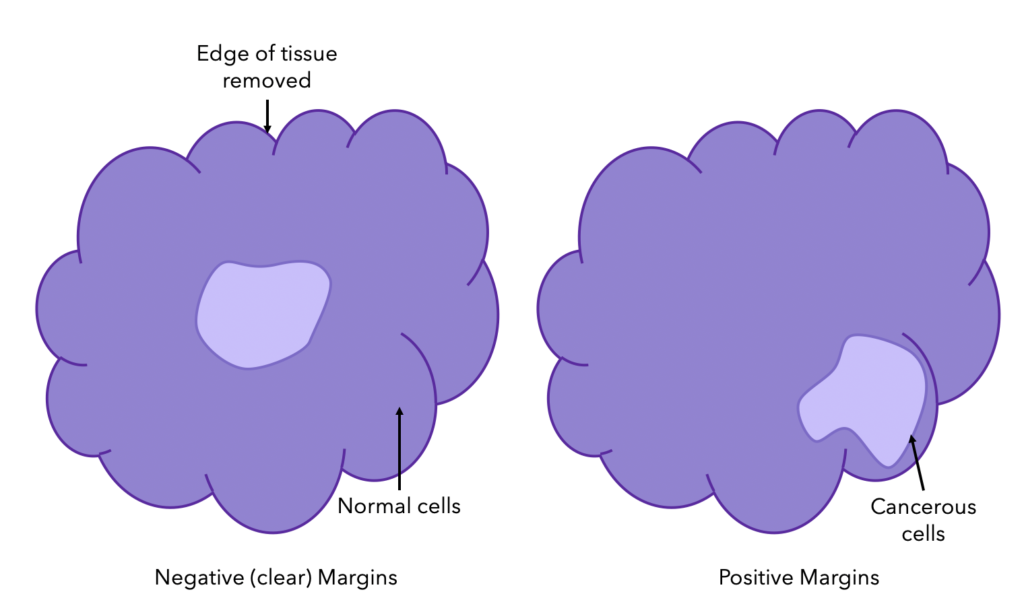
During breast cancer surgery (breast-conserving or mastectomy), the surgeon also takes out a layer of normal tissue surrounding the cancer cells to make sure all the cancer is removed. This layer of tissue is called the margin.
The margin is then tested to confirm that all cancerous cells were removed. If the margin is clear, there are no cancer cells seen; if it is positive, then cancer cells are out to the edge of the tissue, and if it is close, cancer cells are close to the edge of the tissue but not right at the edge (see the diagram below). For both positive and close results, further surgery may need to be considered.
What is the Stage of my cancer?
Staging is the process of combining all the features of your breast cancer to then help decide your treatment plan. It ranges from 0 to 4, and focuses on the size and spread of cancer. It differs from grading as it does not just look at the physical characteristics of the cells. Stage 0 means the breast cancer is non-invasive and therefore has not spread to other tissues within the breast. Stage 4, also known as advanced or secondary cancer, is invasive cancer that has spread from the nearby lymph nodes to different parts of your body. For more information on staging, check out Cancer Research UK’s post.
What is TNM staging?
TNM staging is another indicator of breast cancer’s size and spread. Unlike the staging described above, TNM staging is universal. It’s comprised of T (primary tumour size), N (spreading to nearby lymph nodes) and M (spreading to other parts of the body). Each of these indicators is then further described in terms of advancement. Together they give a detailed explanation of your breast cancer and can be used in deciding the appropriate treatment plan.
We hope you have found this blog insightful and helps you to better understand your pathology report. This series of blogs have been made as part of OWise’s campaign to empower people to better understand their diagnosis and treatment during Breast Cancer Awareness Month.
Using the OWise breast cancer app, you can input details about your treatment and receive a personalised treatment report which can be reviewed at any time and shared with your care team. These reports follow the UK NICE guidelines and can be very helpful for you to understand and explore your treatment plan further. Download the app for FREE today!
References
- Cahill et al., (2017). Rapid virtual hematoxylin and eosin histology of breast tissue specimens using a compact fluorescence nonlinear microscope. Lab Invest. 98(1):150-160.
- National Breast Cancer Foundation. (2020). Breast Anatomy – National Breast Cancer Foundation.
- Cancerresearchuk.org. (2020). Types of breast cancer and related conditions| Breast Cancer | Cancer Research UK.
- Macmillan.org.uk. (2020). Ductal carcinoma in situ (DCIS).
- Cancerresearchuk.org. (2020). Rare types of breast cancer| Breast Cancer | Cancer Research UK.
- Nice.org.uk. (2018). Early and locally advanced breast cancer: diagnosis and management | Breast Cancer | Cancer| Conditions and diseases| NICE Guidance.
- Pathology.jhu.edu. (2020). Staging and Grade | Breast Basics | Explain my results| My Options.
- Campbell et al., (2016). The combined endocrine receptor in breast cancer, a novel approach to traditional hormone receptor interpretation and a better discriminator of outcome than ER and PR alone. British Journal of Cancer. 115: 967–973.
- Li Y, Tsang J, Tam F, Loong T, Tse G. (2023). Comprehensive characterization of HER2-low breast cancers: implications in prognosis and treatment. eBioMedicine. 91:104571.
- FDA. (2022). FDA Approves First Targeted Therapy for HER2-Low Breast Cancer. FDA.
- EMA. (2023). Enhertu. EMA.
