
A prostate cancer diagnosis can turn your world upside down. Not only the prostate cancer diagnosis itself but the results of the multiple tests you will have received, which may be returned to you at different times and in different formats. One example of this is a pathology report which is sent to your doctor to outline the results of a tumour sample. This information can be overwhelming and it can be difficult to process it all. That’s why we have created a comprehensive resource that can be used as a reference to help you better understand the information you have been given.
A pathology report is not always given to you by your clinical team, however it is important to ask your doctor or nurse for a copy, as it can help you better understand your prostate cancer diagnosis and treatment plan. This information is key for you to be able to better discuss with your doctor which treatment suits you best, make informed decisions and ask detailed questions.
Not all reports will include the same amount of information and there may be variation among hospitals in the layout and terms used. This blog provides an outline of the most commonly included aspects of a pathology report but take note that it may not look identical to yours. We also explain the other factors that are considered when diagnosing prostate cancer, outline how the prostate cancer is diagnosed, as well as the procedures that it may involve.
Want to keep track of everything about a prostate cancer diagnosis and treatments in one easily accessible place? With the OWise Prostate Cancer app you can use the diary function to keep a record of all of your appointments, notes, photos and audio recordings in one secure place that can be easily accessed at any time! To learn more about how OWise works, click here.
What is a pathology report?
Pathology is the science that studies the cause and effect of diseases. Pathologists examine tissue samples, in our case the cells that make up the prostate tissue. Specifically, pathologists stain tissue slices from the prostate cancer sample with different markers that they then analyse under the microscope (the diagram below is an example of what they look like). After examining the tissues, the pathologist writes a report about the cancer sample.
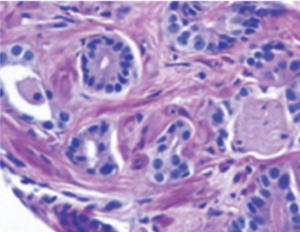
Figure 1: Biopsy image of a prostate tumour [Gleason (4+4)]1
The sample that the pathologist receives may be tissue from a biopsy (tissue sample) or from a radical prostatectomy (surgical removal of the prostate). The amount of detail in each report will depend on what tissue you’ve had removed and how much. There are other types of procedures which doctors may use to get tissue samples such as transurethral resections (TURP). TURP is used to remove parts of the prostate if it is enlarged and causes urinary issues that are not responsive to medication.
There are around 49,000 new prostate cancer cases in the UK every year, that’s around 130 every day.Almost 9 in 10 men with a prostate cancer diagnosis in England survive their disease for five years or more.2
What is a PSA level?
PSA stands for prostate specific antigen and is a type of protein produced by the prostate gland. PSA levels vary between men and are also dependent on age and the size of the prostate. For example, as a guide, a normal PSA level for men in their 50s would be a PSA of up to 3 ng/mL (nanograms per millilitre), for men in their 60s this is raised to 4 ng/mL and for men in their 70s 5ng/mL. There is not a PSA level limit for men aged 80 and over.3
PSA levels are measured through a blood test. A raised PSA alone does not indicate the presence of prostate cancer but this may lead to further tests such as a digital rectal examination (DRE), multiparametric MRI scan (mpMRI) or biopsy.
What is an mpMRI?
A multiparametric MRI (mpMRI) scan is a type of MRI scan. It can provide a more detailed image of your prostate than an average MRI scan, as it combines multiple types of images. Usually you have an mpMRI before a biopsy, as it can help determine whether a biopsy is needed and as a result, a more accurate location from which to remove tumour samples.
What are the different types of biopsy?
There are two main types of biopsies, trans-rectal ultrasound (TRUS) guided biopsy and transperineal biopsy. Most hospitals now routinely use transperineal biopsies and have stopped performing TRUS biopsies.4
- TRUS biopsy takes a sample using a needle going through the wall of the back passage (the rectum).
- Transperineal biopsy the needle goes through the perineum, which is the skin between the testicles and the back passage.
My pathology report mentions cores, what does this refer to?
Multiple samples of the prostate are taken during a biopsy to better understand the location and progression of the prostate cancer – these samples are referred to as cores. Usually at least 10 to 12 samples (cores) are taken to make sure no cancer cells are missed.5
Location of the samples
Often, the location from which samples are extracted is recorded in the pathology report. This will tell you whether the cancer cells were in the left or right, top, middle or bottom of the prostate. This information is important as the location of the cancer can guide treatment options.5
Extent of the cancer
In addition to the number of cores (samples) taken and their location, pathologists will record how many of these cores had cancerous cells and to what extent. This information will be provided as the total number of samples containing cancer, as well as their location (the left or right of the prostate). They will also provide at least one of the following:
- The total percentage of cancer in all the cores combined
- The greatest percentage of cancer in one core
- The longest length of tumour in one core
Whatever the measurement used, your doctor will be able to use this information to determine the likelihood that the cancer is confined to the prostate or that it has spread.5
What is the histological tumour type?
The histological type describes the type of tissue that the cancer originated from. The most common type of cancer is Acinar adenocarcinoma. This means the cancer has originated from acinar cells which are found lining the prostate gland. Rarer types of prostate cancer include ductal adenocarcinoma, which is a cancer that originates in the ducts or tubes of the prostate gland, urothelial cancer, squamous cell cancer and small cell prostate cancer. It is possible to have more than one type of prostate cancer. To find out more about these types, head to the Cancer Research UK website.
Using the OWise prostate cancer app, you can input your profile details and receive a personalised diagnostic and treatment report. You can review this at any time and share it with a member of your care team. Download the app for free today.
What is the Grade of the prostate cancer?
Gleason score and Grade groups are both ways to describe the grade of prostate cancer. You may hear either of these terminologies but they both tell you the same thing – how much the cancer cells look like normal prostate cells.
Gleason Score
The Gleason score is divided into two parts. This is because there is often a wide range of cancer cells within each sample. Therefore, the Gleason score combines the two most common cell types in the sample. Cells are graded between 1-5, with 1 signifying the cancer cells look more like normal cells, and 5 meaning they look the most different from normal cells. The sum of these two scores makes up the Gleason score, which can be between 2 and 10. The first number is the most common type of cancer cell in the sample (primary score), and the second number is the second most common type of cancer cell (secondary score). For example:
- A Gleason score of 7 (3+4) means most cells have a score of 3 (primary score), and the second most common is a score of 4 (secondary score).
- A Gleason score was 7 (4+3) means the most common score of cancer cell was 4 followed by 3.
Grade Group
A grade group means the same thing as a Gleason score, but is documented differently. The grade group can be between 1 and 5. The higher the grade meaning the more irregular the cancer cell compared to normal cells. Please refer to Table 1 to see the direct comparison of grades and Gleason scores.
As an example, a Gleason score of 6 (3+3) is the same as saying that it is a Grade group 1.
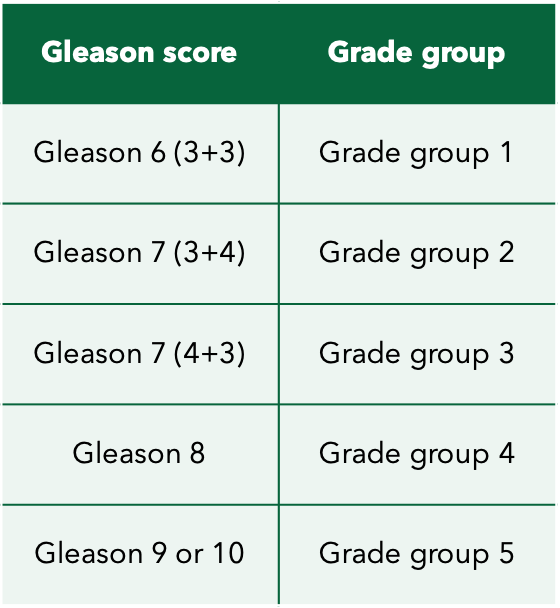
Table 1: Corresponding Gleason and Grade scores
What is TNM staging?
TNM staging is an indicator of the prostate cancer’s size and spread. It consists of T (size and location of primary tumour relative to prostate size), N (spreading to nearby lymph nodes) and M (spreading to other parts of the body). Each of these indicators is then further described in terms of advancement. Together they give a detailed explanation of the prostate cancer and are used for diagnosis and deciding the appropriate treatment plan. You can find explanations of all the different TNM scores used in the OWise app.
What is the T stage of the tumour?
As mentioned above, the T stage describes the size and location of the primary tumour relative to the size of the prostate. You can find the different T stages described below:
- T1: Cancer too small to be seen on a scan or felt during examination of the prostate.
- T1a: Cancer is less than 5% of the removed tissue. These are found unexpectedly during surgery for other reasons.
- T1b: Cancer is more than 5% of the removed tissue. These are found unexpectedly during surgery for other reasons.
- T1c: Cancers are found by biopsy after suspicion of potential cancer, for example after a raised PSA level.
- T2: Cancer is completely contained inside the prostate gland.
- T2a: Cancer is only in half of one side of the prostate gland.
- T2b: The cancer is in more than half of one side of the prostate gland, but not both sides.
- T2c: The cancer is on both sides but is still inside the prostate gland.
- T3: The cancer has broken through the covering of the prostate gland.
- T3a: The cancer has broken through the covering of the prostate gland but has not spread into the tubes that carry semen.
- T3b: The cancer has spread outside the capsule (covering) of the prostate gland and into the tubes that carry semen (seminal vesicles).
- T4: Cancer has spread into other body organs nearby, such as the back passage, bladder, or the pelvic wall6.
What type of prostate cancer do I have?
Localised
Localised prostate cancer refers to the cancer remaining completely inside the prostate gland. It has not spread to any tissues surrounding the prostate nor to other organs around the body. Localised prostate cancer is typically divided into three categories: low risk, intermediate risk and high risk. These categories are determined by your PSA level, Gleason score/Grade group and TNM stages.
- Low risk localised prostate cancer means the cancer has not spread out of the prostate gland, and it is not likely to spread or grow much if at all. This type of prostate cancer may not need treatment and can be monitored instead. This is defined by having the following:
- PSA <10 ng/mL and
- Grade group 1 or Gleason 6 and
- T1 to T2a
- Intermediate risk localised prostate cancer has also not spread out of the prostate, but has an intermediate risk of spreading in the future. However, it is unlikely to grow for at least a few years. This is defined by having the following:
- PSA 10-20 ng/mL or
- Grade group 2-3/Gleason 7 or
- T2b
- High risk localised prostate cancer is also still contained within the prostate, but it has a high risk of spreading which means it may spread within a few years. High risk localised prostate cancer can also be referred to as a locally advanced prostate cancer. This is defined by having the following:
- PSA >20 ng/mL or
- Grade group 4-5/Gleason 8-10 or
- T2c
Locally advanced prostate cancer
Locally advanced prostate cancer means the cancer has broken the covering surrounding the prostate, referred to as the capsule, and has spread to surrounding tissues (N1). This can include the tissue around the prostate, the tubes that carry semen (seminal vesicles), body organs nearby such as the back passage (rectum) or neck of the bladder, or lymph nodes close to the prostate gland.
Advanced prostate cancer
Advanced prostate cancer, also known as metastatic prostate cancer, means that the cancer has spread to other parts of the body (M1). It most commonly spreads to the lymph nodes in other parts of the body or to the bones, however it can also spread to other organs.
How do I know if the prostate cancer has spread to my lymph nodes?
Prostate cancer cells often first spread to the lymph nodes in your pelvic region (pelvic lymph nodes). Lymph nodes are a network of small glands throughout your body that help you fight infection. A diagnostic biopsy will not normally remove any lymph nodes. The presence of prostate cancer in lymph nodes will usually be investigated in other types of surgeries, namely radical prostatectomies (removing of the prostate). Another way doctors check whether prostate cancer has spread to your lymph nodes is a CT scan.
If the prostate cancer has spread into your lymph nodes, your doctor may recommend a lymphadenectomy (which is also called lymph node dissection). This is a surgical procedure which removes one or several of your lymph nodes. In prostate cancer, it is usually the pelvic lymph nodes which are removed.
What is lymph-vascular invasion?
The lymphatic vessels are part of the lymphatic system, which is a network of tissues and organs (lymph nodes) that help get rid of the body of toxins, waste and unwanted materials. If your report mentions lympho-vascular invasion, it means that the cancer cells have reached these vessels and have a higher chance of spreading to other parts of the body.
The OWise prostate cancer app can assist you with your treatment or pathway options through a personalised “Decision aid” tool. This involves answering a short set of questions to evaluate your personal preferences in relation to the various side effects of different treatments. This shared-decision making tool can be used to assist you in better conversations with your care team.
What is perineurial invasion?
Within the prostate there is a nerve fibre. If prostate cancer cells are surrounding or growing inside this, then it is termed as perineural invasion. This means that there is a higher chance that the cancer has spread outside the prostate. However it does not mean for certain that the cancer has spread, other factors such as the Gleason score will also have an effect on the risk of spreading. Still, it is best to discuss the findings of this with your doctor.7
Has the prostate cancer spread to the seminal vesicles?
The seminal vesicles are glands near the prostate that provide part of the fluid in semen. If you undergo a radical prostatectomy (surgical removal of the prostate) it is common for the seminal vesicles to be removed and checked for cancer by the pathologist. Seminal vesicle invasion (SVI) means prostate cancer has spread to the seminal vesicles. Your treatment plan will differ depending on if cancer cells have spread to your seminal vesicles because there is an increased chance of cancer recurrence.8,9
What is extraprostatic extension?
Extraprostatic extension (or EPE) means cancer cells have spread outside of the prostate. It is sometimes referred to as extracapsular extension. This is sometimes detected through an mpMRI, or through a prostate biopsy, though most often this is found through radical prostatectomy. Seminal vesicle invasion is a type of extraprostatic extension.10,11
If I have had surgery, are the margins clear?
After surgery, your prostate is sent to a laboratory to be looked at by a pathologist. The pathologist will inspect the edges of the tissue removed; this layer of tissue is called the margin. The margin is then tested to confirm that all cancerous cells were removed.
- Positive margins suggest that not all of the cancer cells were removed and further treatment may be considered.
- Negative margins suggest that all of the cancer cells were removed.
- Close margins suggest that some of the cancer cells may be left behind and further treatment may be considered.
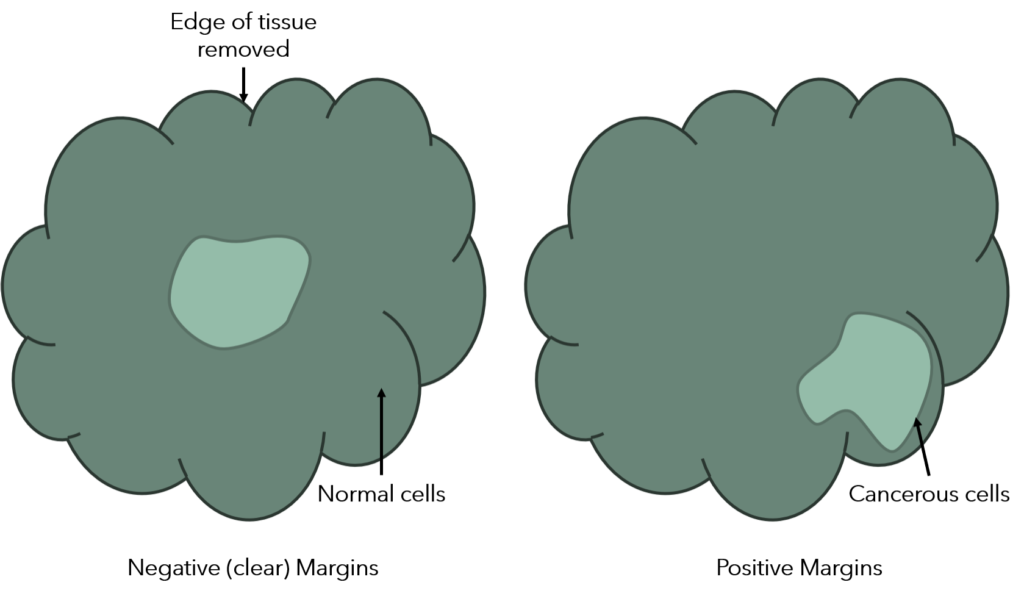
Figure 2: Diagram of surgical margins
It is a good idea to discuss the results of the margin examination with your doctor, so you may want to ask them about this at your first follow-up appointment after surgery.
Familial prostate cancer and BRCA risk testing
A family history of cancer can increase the risk of developing prostate cancer. One of the most well known genes responsible for this is BRCA. If you have a family history of prostate, breast or ovarian cancer, you can be offered a BRCA genetic test through the NHS.
There are other special tests that the pathologist sometimes uses in order to help determine a prostate cancer diagnosis. Not all patients need these tests. Whether or not your report mentions these tests has no effect on the accuracy of your diagnosis.
We hope this blog can be a helpful resource to better understand your pathology report and a prostate cancer diagnosis. There are a few different ways to categorise and measure prostate cancer: Gleason scores, Grade groups, TNM staging – all of which we have unpacked and outlined in this blog. All of these factors will be considered by doctors when discussing treatment options with you.
We hope you have found this blog insightful and that it helps you better understand your pathology report and a prostate cancer diagnosis.
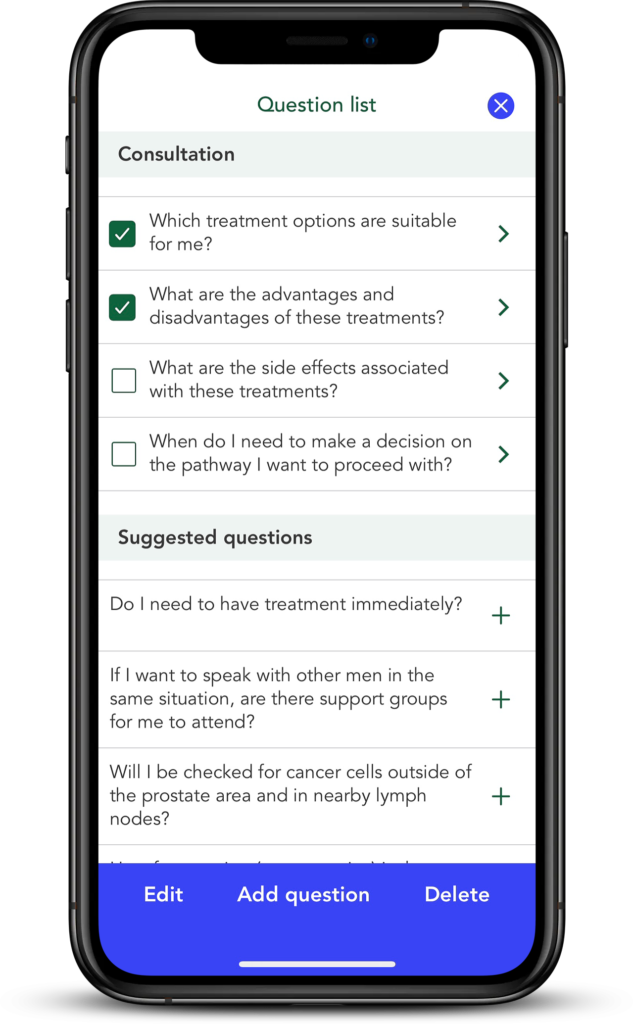
If you have any questions about your pathology report or a prostate cancer diagnosis, make sure to note them down using the Question lists feature of the OWise app. This way, you can remember to ask all of your questions at your next appointment and you have space to write down or record the answers for future reference.
References
- B. Turkbey et al., (2011) Documenting the location of prostate biopsies with image fusion. BJU Int., vol. 107, no. 1, pp. 53-57.
- Cancerresearchuk.org. (2020). Prostate cancer statistics | Cancer Research UK. [online] Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer
- Macmillan Cancer Support. PSA test. [online] Available at: https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/psa-test
- Prostate Cancer UK. (2021) Prostate biopsy. [online] Available at: https://prostatecanceruk.org/prostate-information/prostate-tests/prostate-biopsy
- Oxley, et al., (2016) Dataset for histopathology reports for prostatic carcinoma. The Royal College of Pathologists.
- Cancerresearchuk.org. (2020). TNM Staging | Cancer Research UK. [online] Available at: https://www.cancerresearchuk.org/about-cancer/prostate-cancer/stages/tnm-staging
- Ström P, et al., (2020) Prognostic value of perineural invasion in prostate needle biopsies: a population-based study of patients treated by radical prostatectomy. Journal of Clinical Pathology. 73:630-635.
- Dr Joachim Feger and Dr Paresh K Desai et al. Extraprostatic extension of prostate cancer. [online] Available at: https://radiopaedia.org/articles/extraprostatic-extension-of-prostate-cancer?lang=gb
- Fleshner K, Assel M, Benfante N, et al. Clinical Findings and Treatment Outcomes in Patients with Extraprostatic Extension Identified on Prostate Biopsy. J Urol. 2016;196(3):703-708.
- Potter SR, Epstein JI, Partin AW. Seminal vesicle invasion by prostate cancer: prognostic significance and therapeutic implications. Rev Urol. 2000;2(3):190-195.
- Dr Joachim Feger. Seminal vesicle invasion. [online] Available at: https://radiopaedia.org/articles/seminal-vesicle-invasion?lang=gb
