Chemotherapy (often called chemo) is a common treatment for breast cancer. While chemotherapy can be an effective treatment option, it can also be daunting and overwhelming for patients who may not know what to expect during the process. Let’s take a look at how chemotherapy works, the different types and what to expect when receiving your treatment. Here you can find some useful tips that will help you to manage potential side effects, know how to prepare for your treatment and what to expect during follow-up appointments. All information in this blog is based on reliable scientific resources.
How does chemotherapy target breast cancer cells?
The function of chemotherapy drugs is to stop the tumour from growing and prevent spreading of cancer cells to other parts of the body1. For tissue to grow, cells need to divide. In cancer, cells continue to divide and accumulate until they form a cluster of cells known as a lump or tumour. To stop the tumour from growing, chemotherapy interferes with dividing cells. This interference can take place at different stages within the cell division process. Chemotherapy drugs cause changes in the genetic material (DNA) and proteins of cancer cells, leading to cell death2. For a cell to divide, it needs to duplicate its DNA. Chemotherapeutic drugs can, for example, prevent the production of new DNA molecules or stop proteins that form ‘the machine’ that copies the DNA3. Interference with the DNA of the cells leads to cell death and thus prevents the cell from multiplying (figure 1).
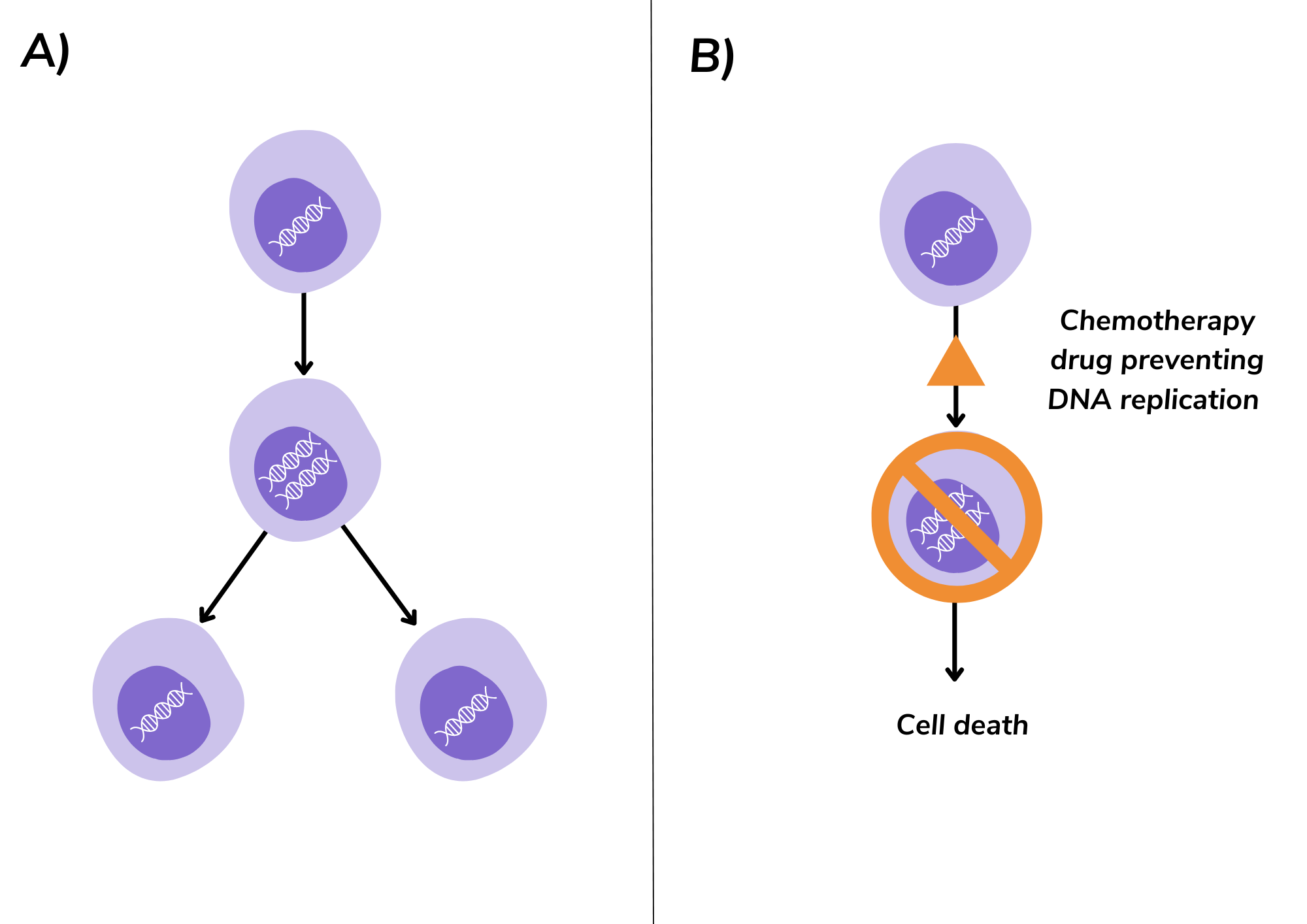
Figure 1. The effect of chemotherapy on dividing cells A) The normal cell division process: DNA in the middle of the cell is multiplied and then split into two new cells. B) Certain chemotherapy drugs interrupt the cell division process by preventing DNA replication, leading to cell death.
Are all chemotherapy drugs the same?
There are multiple chemotherapy drugs to treat breast cancer. During chemotherapy, patients commonly receive two or more different drugs. These drugs are specifically chosen to damage the cells at different stages of the cell division process. Using a combination increases the chance of killing a larger number of cells.
How does chemotherapy affect healthy cells?
Chemotherapy targets rapidly dividing cells non-specifically, meaning it can also destroy healthy fast-dividing cells. As it travels through the bloodstream it can impact fast-dividing cells throughout the whole body. Normal fast-dividing cells in our bodies include white blood cells, bone marrow and cells in the hair follicles, nails, mouth and digestive tract. The cytotoxic effect of chemotherapy on these healthy cells can commonly result in side effects such as hair loss, changes to nails, mouth sores, diarrhea, nausea and vomiting. However, healthy cells are generally more capable of recovering and repairing themselves compared to cancer cells. This means that most side effects are temporary, can be managed with medication and will resolve after you finish your treatment. Many patients have told us they find it useful to track their side effects in the OWise app, as it can really help to share the detail in discussions with their care team.
When do you get chemotherapy for breast cancer?
Chemotherapy can be given for both primary and secondary breast cancer. For primary (early-stage) breast cancer, a chemotherapy regimen combining two to three drugs is usually recommended. Drugs are often combined as each chemotherapy drug can affect cancer cells in a different way. For secondary (also called metastatic or advanced) breast cancer, chemotherapy can often be prescribed as a single drug. However, there are some combinations that can be used to treat advanced breast cancer. Chemotherapy can be given in the following situations:
Neoadjuvant chemotherapy (before surgery or radiotherapy)
This is chemotherapy given to you before your main treatment, which is usually surgery or radiotherapy. The goal is to reduce the size of the tumour and lower the risk of cancer coming back3. Shrinking the tumour through chemotherapy makes it possible to have less surgery and, in the case of radiotherapy, it may be possible to have radiotherapy to a smaller area of the body4. It may also be used this way to understand if the cancer cells “repond” to the treatment and die. Neoadjuvant therapy may be recommended to people with HER2-positive, triple negative, breast cancer (BRCA) gene-positive, high risk or inflammatory breast cancer.
For more on neoadjuvant treatment, take a look at The concept of neoadjuvant treatment blog.
Adjuvant chemotherapy (after surgery or radiotherapy)
Adjuvant chemotherapy is given after your initial treatment, such as surgery or radiotherapy. It can suppress or kill the growth of cancer cells that may have been left behind after your initial treatment1. It prevents any remaining cells from spreading and lowers the risk of the cancer returning.
For breast cancer that has spread
As well as treating primary breast cancer or breast cancer that has recurred, chemotherapy can be used to treat breast cancer that has spread to other parts of your body (also called secondary, metastatic, or advanced breast cancer). When surgery is not possible, chemotherapy can serve as the main treatment for secondary breast cancer. It can be used in combination with targeted therapy for HER2-positive disease, or immunotherapy, to enhance its effectiveness. In cases of secondary breast cancer that is incurable, the goal of chemotherapy is to improve quality and duration of life.
For more information on secondary breast cancer check out the blog Secondary breast cancer: pathology, signs and diagnosis.
Types of chemotherapy for breast cancer
What is taxane chemotherapy?
Taxanes, like docetaxel or paclitaxel, are one of the most common chemotherapy drugs available for both primary and secondary breast cancer. They can be offered individually or combined with other chemotherapeutic agents, such as those mentioned below. Taxanes bind to structures in the cell that are essential for cells to divide and thus to grow. The binding of a taxane blocks the function of these cell structures and the DNA that is copied can no longer be separated which will lead to cell death. This is how taxane chemotherapy slows the growth of fast-dividing cells, including cancer cells, and kills them. Researchers found that adding a taxane drug to chemotherapy enhances survival rates and decreases the chance of cancer coming back compared to chemotherapy without taxanes5.
What are anthracyclines?
Anthracyclines, such as doxorubicin or epirubicin, are described as “anti-tumour antibiotics”. They work by binding to the DNA inside the cells, and by interfering with the DNA they prevent them from multiplying further2. This will slow the growth of rapidly dividing cells, including cancer cells, and kill them. These drugs are given via the bloodstream and can be used to treat both primary and secondary breast cancer patients.
Anthracyclines can be cardiotoxic, meaning they can have a damaging effect on the heart. Therefore, if people are not suitable for anthracyclines (because of previous treatment or the toxicity to the heart) other treatments options are available. Every chemotherapy drug can come with a whole range of side effects. This is why it is important to be able to monitor these and share any changes with your doctor.
Do you know that you can track your side effects with OWise? With more than 30 side effects and symptoms to choose from, you can track any changes and share these with your care team and loved ones via a secure hyperlink. Having better communication with your care team can ensure you receive the best care possible.
What are antibody-drug conjugates?
An antibody-drug conjugate (ADC) is a relatively new class of chemotherapy, which targets specific cancer cells. An ADC is a monoclonal antibody (such as trastuzumab) directly linked to a chemotherapy drug. It helps the chemotherapy drug find the cancer cells more effectively, as the monoclonal antibody targets and binds to the cell and the chemotherapy drug becomes active as it enters the cell. This allows chemotherapy to be more targeted and lessens its effect on non-cancer cells.
Currently, both trastuzumab emtansine (T-DM1 or Kadycla®) and trastuzumab deruxtecan (Enhertu®) are approved by NICE for people with secondary HER2-positive breast cancer after having had at least one line of treatment with an anti HER2-chemotherapy combination6,7. For treating unresectable triple negative advanced breast cancer, the ADC sacituzumab govitecan (Trodelvy®) is recommended after two or more systemic therapies, at least one of which was for advanced disease8.
How is chemotherapy given for breast cancer?
Chemotherapy can be given in various ways depending on the type of breast cancer and type of drugs you are receiving. Your doctor will discuss the option that is most suitable in your situation. The most common ways of having chemotherapies are directly into the bloodstream (intravenously) or taking them in the form of tablets or capsules, also known as oral administration. Let’s take a look at these in more detail.
Via the bloodstream
During intravenous administration the chemotherapy drug is directly delivered into your bloodstream. The chemotherapy can be given intravenously in different ways, for example via:
- A cannula – a small tube which is inserted into a vein in your hand or lower arm9.
- A central line, also known as a central venous catheter (CVC). This is a long thin tube inserted into a vein and directed towards a large vein in the chest, close to the heart. A PICC line and portacath are two common types of central lines9.
- PICC line – a thin tube which runs up a small vein inside your arm and ends into the large vein close to the heart.
- Portacath – a small reservoir implanted under the skin. The port is connected to a line placed into the large vein close to the heart. The portacath is invisible from the outside of your body.
Once your cannula, line or port is in the right position, chemotherapy drugs can be administered into the body through injection or infusion (as a drip).
Orally
Chemotherapy that can be swallowed is available in various forms such as tablets, capsules and liquid. Capecitabine (Xeloda®) is an example. Oral chemotherapy medications have a protective coating that dissolves in the stomach. The released medication is absorbed through the stomach lining. Some medications have unique coatings for delayed or extended release. This allows longer time intervals between the doses. It is important to follow the instructions your doctor or nurse will give you about the type of chemotherapy you will receive. They will explain to you when to take the medication, how often to take it and any special instructions such as if there is anything you should not eat while taking them.
What to expect at the different stages of chemotherapy
What to expect before receiving chemotherapy for breast cancer?
When you are diagnosed with cancer, you will meet with your oncologist and a team of experts will be involved to provide best care. The experts in your care team will advise chemotherapy if they believe it is the most suitable choice. However, it is important to realise that your voice and preferences play a crucial role in determining your treatment plan.
Normally, chemotherapy is given in cycles. Each cycle includes a chemotherapy session and a rest period. A full treatment of chemotherapy consists of multiple cycles, which is called a regimen. The duration of each regimen and total time required to complete depends on the type of chemotherapy medicines you get. Generally, a regimen takes about three to six months10. Your doctor will suggest a chemotherapy treatment regimen including details about the duration of each cycle and the advantages and side effects.
Tips for before you receive chemotherapy for breast cancer
- All information you receive after being diagnosed can be quite overwhelming. Make a list of questions and concerns you have for your care team. You could think about questions on possible side effects, the effectiveness of the treatment and what other options are available. The OWise app can help you with this as it contains suggested questions that can help you prepare for your appointments.
- It is important to let your doctor know about the other medicines, vitamins and supplements you take. This is because there are some medications and foods that can interact with chemotherapy and can have a negative effect treatment
- If relevant, discuss your fertility preservation options with a fertility specialist or counsellor
- Talk to others about the support you will need for things like transportation to chemotherapy appointments, chores and child/pet care. Also think about joining a support group.
- If you are working, you can talk to your employer about how much time you will need off and if it is possible to work flexible hours.
- Increasing your physical fitness before starting chemotherapy treatment improves your tolerance of the treatment and is associated with higher chemotherapy completion rates
What to expect while receiving chemotherapy for breast cancer?
There are different places at which you can receive chemotherapy. You can receive chemotherapy in a hospital, doctor’s office or an infusion centre. Before receiving chemotherapy, some measurements will be done to check your health, such as measuring your blood pressure, pulse and temperature, and a blood sample will be taken to count the amount of red and white blood cells in your blood10,11. Your height and weight will be measured to determine the right dose of chemotherapy.
Prior to receiving chemotherapy, it is possible to get some pre-chemotherapy medicine to prevent an allergic reaction or nausea. Next to this, fluids can be given to improve the function of specific chemotherapy drugs. After everything is checked and ready, the chemotherapy infusion process will start. The duration of your treatment session will vary based on several factors. Some chemotherapy treatments take minutes or hours while others may be spread out over several days or weeks (continuous infusion). In case of continuous infusion, you do not have to stay at the hospital or clinic. The chemotherapy is given via a small pump you can wear or carry.
Tips for when you are receiving chemotherapy for breast cancer
- Pack a bag to take with you to your appointments that includes food and things to pass the time
- Wear comfortable clothes and shoes
- Drink plenty of water to stay hydrated
- Keep track of treatment plan and side effects with the OWise app
What to expect after receiving chemotherapy for breast cancer?
When the treatment is finished, your blood pressure, pulse and temperature will be checked again. Your doctor or nurse will talk to you about the possible side effects and how to manage them.
Tips for after you have received chemotherapy for breast cancer
- To help the chemotherapy move through- and get removed from the body, it is advised to drink plenty of water for at least 48 hours after the treatment.
- Avoid people who have a cold or other infections. As chemotherapy weakens your immune system, it is more difficult for your body to fight infections.
- Ask your doctor or nurse who you can reach out to in case you have any questions or concerns, including contact details for after hours or weekends.
- You can read more about moving forward after finishing your treatment and managing concerns in this OWise blog.
And that’s chemotherapy for breast cancer summed up
We hope that this blog helped you to get a better understanding of how chemotherapy works and gave some valuable insights into your treatment journey and options. By knowing what to expect during your chemotherapy sessions, you can approach them with more confidence. Remember that you are not alone in this journey, your health care team is there to support you during each step. By being well-informed and proactive, you can work towards achieving the best possible outcome for your health and well-being.
This blog is the first of our new series on chemotherapy, where we will cover different side-effects, patient experiences and the latest developments in the field. So, stay tuned for the upcoming blog posts. At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Twitter for any updates. Any questions? Get in touch!
References
- Muhammad T. Amjad, Anusha Chidharla, Anup Kasi. Cancer Chemotherapy. Fundamentals of Pharmaceutical Nanoscience [online]. 2023 Feb 27;401–27. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564367/
- Falzone L, Bordonaro R, Libra M. SnapShot: Cancer chemotherapy. Cell. 2023 Apr 13;186(8):1816-1816.e1
- National Cancer Institute. NCI Dictionary of Cancer Terms: neoadjuvant therapy [online]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/neoadjuvant-therapy
- Cancer Research UK. 2020. When you might have chemotherapy | Cancer in general [online]. Available from:https://www.cancerresearchuk.org/about-cancer/treatment/chemotherapy/when-you-might-have-chemotherapy
- Willson ML, Burke L, Ferguson T, Ghersi D, Nowak AK, Wilcken N. Taxanes for adjuvant treatment of early breast cancer. Cochrane Database Syst Rev [online]. 2019 Sep 2;2019(9). Available from: https://pubmed.ncbi.nlm.nih.gov/31476253/
- NICE. 2017. Trastuzumab emtansine for treating HER2-positive advanced breast cancer after trastuzumab and a taxane | Guidance | NICE [online]. Available at: https://www.nice.org.uk/guidance/ta458/chapter/1-Recommendations
- NICE. 2023. Trastuzumab deruxtecan for treating HER2-positive unresectable or metastatic breast cancer after 1 or more anti-HER2 treatments | Guidance | NICE [online]. Available at:https://www.nice.org.uk/guidance/ta862/chapter/1-Recommendations
- NICE. 2022. Sacituzumab govitecan for treating unresectable triple-negative advanced breast cancer after 2 or more therapies | Guidance | NICE [online]. Available at: https://www.nice.org.uk/guidance/ta819/chapter/1-Recommendations
- Cancer Research UK. 2020. Central lines | Cancer in general [online]. Available from: https://www.cancerresearchuk.org/about-cancer/treatment/chemotherapy/how-you-have/into-your-vein/central-lines
- Breastcancer.org. 2022. What to Expect During Chemotherapy Treatment [online]. Available from: https://www.breastcancer.org/treatment/chemotherapy/what-to-expect
- Cancer.Net. 2021. What to Expect When Having Chemotherapy [online]. Available from: https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/what-expect-when-having-chemotherapy
