
Breast cancer and its treatments can result in significant and lasting changes to your body and it’s unsurprising that your sex life may change along with it. While for some, these changes may be minimal and temporary, for others the frequency, quality and duration of intimate moments with a partner, or yourself, can be very different to those prior to treatment. A study with over 800 participants found that a third of breast cancer patients felt some kind of negative impact on their sex life, and most agreed that it had changed in one way or another ¹.
In this blog we’ll look at the different kinds of treatment that can cause these changes, and then examine the changes themselves. Whether you’re more fatigued now than you were, or pain is discouraging you from the bedroom, we’ll look at the various symptoms associated with an altered sex life and ways of managing them.
So, how can breast cancer treatments affect Sex and Intimacy?
Most breast cancer treatments can act as an impediment to sex and intimacy, so it’s worth examining how they cause or exacerbate certain symptoms. The main culprits are surgery, hormone therapy, chemotherapy and radiotherapy which each have unique effects:
Surgery
While many different kinds of treatment can have an effect on sex and intimacy, the one that might appear to be the most obvious is surgery. Beyond the pain and discomfort that comes directly after an operation like a mastectomy, breast-conserving surgery or lymph node removal, there can be further barriers to enjoying sex and intimacy. This can include a prolonged sense of pain due to nerve damage during the operation, a lack of sensitivity that would normally be pleasurable during sex, as well as issues associated with body image.
Hormone Therapy
Hormone therapies can have varying effects on your body. For those therapies that limit the amount of circulating oestrogen, this may cause some menopausal symptoms such as hot flushes, night sweats and vaginal dryness – all of which can act as barriers to your normal sex life. Joint pain, which is prevalent among those using aromatase inhibitors for example, can also make sex more challenging.
Chemotherapy
Chemotherapy can take a big toll on your body as this treatment can affect both cancer cells and normal healthy cells, and it isn’t possible to tell beforehand which side effects you’ll experience. Some of the side-effects that can impact on your sex life include fatigue, nausea, hair loss and the same menopausal symptoms associated with hormone therapy.
Radiotherapy
Following radiotherapy, there may be some time where the targeted area is sore or tender meaning that touching yourself or being touched by a partner can be very painful. Even if this is just for a short time during recovery, it can still be a distressing issue.
A recent study in the Netherlands showed that cancer patients felt they would benefit from receiving personalised information about the potential impact of treatment on their sexual health from their doctors, both during and after treatment ¹¹.
Having “The Conversation”
Before going into detail about the different symptoms caused by these treatments, it’s important to know who to speak to about any issues you might have. It might be a good idea to have a conversation with your partner, outside of the bedroom, about how you are feeling, any changes you may be experiencing and how your sex life may now be different from beforehand. That way you’ll both be on the same page and you’ll have a better idea of what to expect.
While keeping a healthy dialogue with your partner about how your feelings of sex and intimacy change is one thing, speaking up about this topic with your care team can be just as important. However, as we shall see, this topic can be suspiciously absent at the doctor’s office. According to one study, only 30% of couples spoke to their doctor about sexuality and how it would be affected by cancer ², and this may be down to poor communication on the part of the doctor.
A report published by Breast Cancer Now entitled, ‘My Body, Myself’, shows how the topic of sexual health was rarely brought up, and in the cases where it was, it was not raised as a serious issue. Here are a few accounts from some of the participants:
“It is as if they are only concerned with the physical treatment of the cancer, and that you are almost being vain if you care about any of the rest” — Rachel, 47.
“I was told about changes to my body but wasn’t offered support” — Jennifer, 40.
It can be daunting to bring up a personal topic like this in front of your GP or oncologist, but speaking up about the concerns you have surrounding sex and sexual health, and asking for help with this can make all the difference. These conversations can help you identify one of the symptoms that we are about to discuss that might be acting as a barrier to a healthy and comfortable sex life. Creating that dialogue is key.
Managing your symptoms
Vaginal Dryness or Irritation
Treatments like hormone therapy can lead to menopausal symptoms, even if you wouldn’t normally expect these symptoms at a young age.
As well as symptoms like night sweats, hot flushes and joint pain, a drop in the oestrogen hormone can have some impact on the vagina. This is because the hormone oestrogen plays a role in maintaining the moisture and elasticity of the vagina, and so a significant decrease in oestrogen levels can cause sex and intimacy to become more painful and uncomfortable than usual, and make reaching orgasm more challenging.
Before addressing the various methods of managing vaginal dryness, it’s important to recognise that sex and intimacy do not always have to revolve around the vagina, in the same way that it doesn’t have to be breast-centric either. It’s all about adapting to what feels comfortable during and after your treatment.
There are a number of products that can provide both short and long-term relief for those experiencing vaginal dryness. Vaginal lubricants can be used during sex or masturbation to reduce friction and temporarily ease any of the pain with vaginal sex, while vaginal moisturisers on the other hand can have much longer-term reduction in discomfort if regularly applied to the area. Topical hormone treatment, in the form of gels or creams, can be applied directly to the vagina to boost oestrogen in the area. However, for this option please speak with your doctor, as this may be unsuitable for those using other hormone treatments such as aromatase inhibitors ³.
As well as trying these products, you can also encourage blood flow to this area by doing some pelvic floor exercises which you can find more about on the NHS Website.
 Finally, when it comes to being intimate with a partner, it’s easier to communicate what feels comfortable to you in the bedroom once you’ve found out for yourself. Self-exploration through masturbating using a vibrator or a vaginal dilator can help you learn what your new limitations are, and which areas are most comfortable to you. Make sure to use products that are skin safe like silicone, glass or metal rather than latex or rubber. Whether privately or with a partner, stimulation in this area can help promote blood flow to your vagina and help maintain its suppleness and elasticity.
Finally, when it comes to being intimate with a partner, it’s easier to communicate what feels comfortable to you in the bedroom once you’ve found out for yourself. Self-exploration through masturbating using a vibrator or a vaginal dilator can help you learn what your new limitations are, and which areas are most comfortable to you. Make sure to use products that are skin safe like silicone, glass or metal rather than latex or rubber. Whether privately or with a partner, stimulation in this area can help promote blood flow to your vagina and help maintain its suppleness and elasticity.
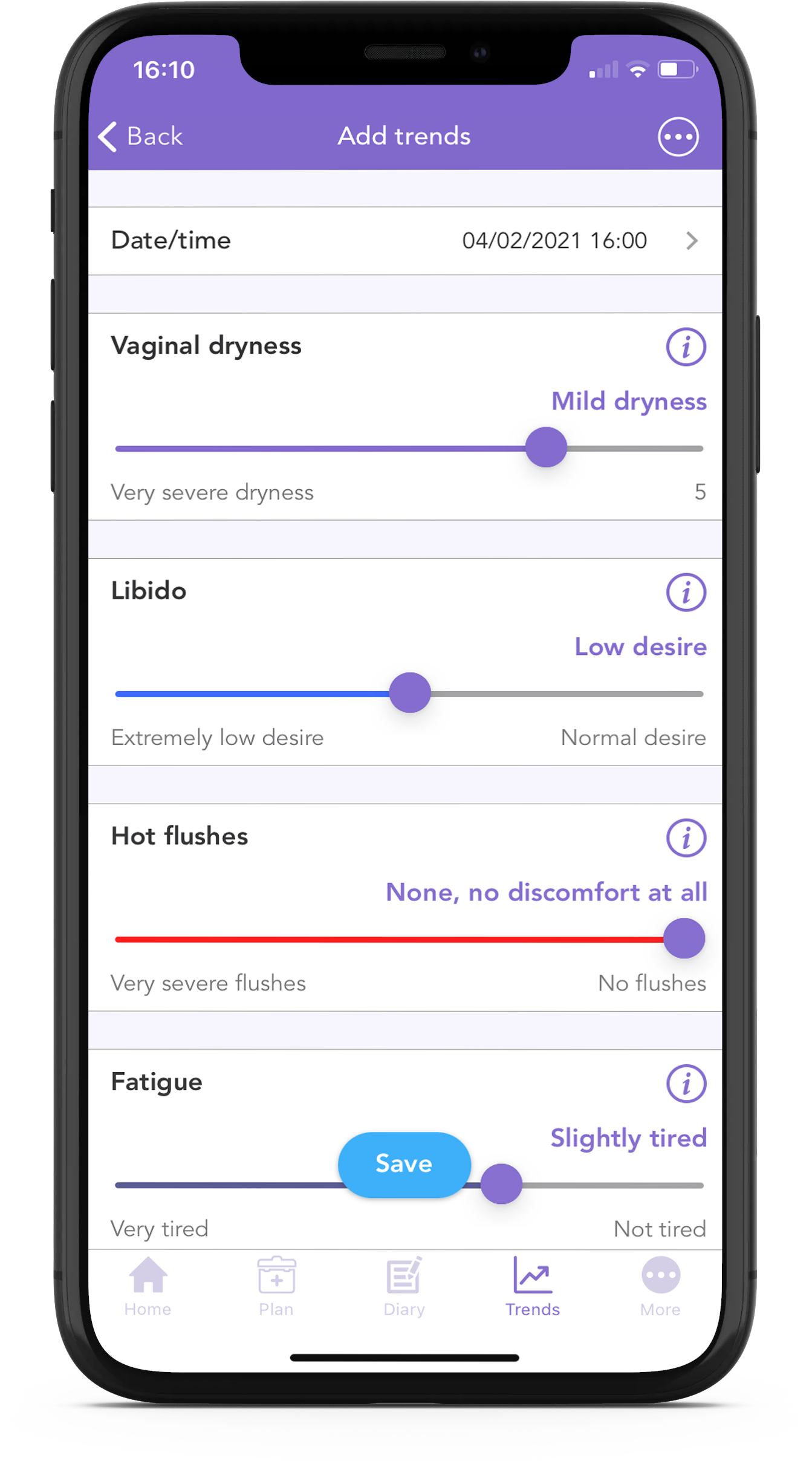
Did you know you can track vaginal dryness and libido using the OWise breast cancer app? The trends feature allows you to input how you’re feeling each day and you can later review how your wellbeing or symptoms have changed over time. The OWise app is absolutely free and you can even share the results with your partner or with someone from your care team.
Pain and Numbness
Breast cancer treatment can cause pain and numbness in different areas around the body and due to different reasons. These changes in sensation can have a direct effect on sex and intimacy.
For women who take aromatase inhibitors, such as anastrozole, letrozole, and exemestane, a commonly experienced symptom is joint pain. This can be experienced in a variety of locations, but most commonly in the fingers, wrists, shoulders, knees and ankles ⁴. If you are taking aromatase inhibitors and want to find out more about the cause and management of joint pain, head to our this blog.
Joint pain can make certain positions uncomfortable during sex. If this is something you are experiencing, there are multiple strategies that can help ease discomfort and pain to make sex more pleasurable. Different positions can be tried out, with the use of pillows or different pieces of furniture to support you. Try to experiment! The positions you are used to may cause strain on your joints and new ones may be more beneficial. It is important to be open with your partner for what works best for you and reach mutual understanding of each other’s needs. (Sex, relationships and arthritis | Starting a family (versusarthritis.org))
After surgery, there may be a few weeks where the area is feeling sore and the arm stiff. This usually subsides, however for some women the pain continues due to nerve damage that occurred during the surgery. Radiotherapy and chemotherapy may also cause pain or numbness during and for subsequent weeks after treatment. In all these cases, patience and dialogue are needed. It may be that you would prefer to refrain from sexual activities until these symptoms have passed, or you may look at alternative forms of intimacy that would not include the affected area. It may also be the case that you want to plan ahead before getting intimate.
Fatigue
Fatigue is one of the most commonly reported symptoms by breast cancer patients, and this can certainly make a change to your regular sex life. Cancer related fatigue, usually a result of chemotherapy or radiotherapy, is unlike usual fatigue in that it isn’t remedied by resting or sleeping. It’s clear from research conducted in this field that fatigue is not limited to the treatment period as it can linger beyond the end date:
“Fatigue typically improves in the first year following treatment completion, although 25–30% of patients continue to experience fatigue for years after successful treatment” ⁵.
While it is known that these two symptoms are clustered together, meaning that they are often experienced at the same time, the specific link is under review by scientists ⁶. However, it has been suggested that there is a vicious cycle where fatigue can cause a drop in libido and vice versa ⁷, though the precise link between these two symptoms is still under review by scientists. In any case, cancer related fatigue may leave you with less spare energy to engage in sex as much as (or in the same way as) you’re used to, and it may take some time to adjust to this.
There are a number of ways of managing fatigue though remember that not every method is equally effective for everyone. Give them all a go and see which works best and which helps your sex life improve the most.
One way to improve cancer related fatigue is by keeping a regular schedule. Whether this means having a rigid sleep schedule, or planning time in the day to take a rest or a nap, having a consistent timetable has been shown to reduce fatigue. Keeping a regular exercise routine has also been shown to be effective, even if the exercise is not too intense, as this generally helps to improve energy levels and sleep quality. It will also have the added benefit of lifting your mood which can be important when considering sex and intimacy. Finally, nutrition can play a key role in keeping fatigue to a minimum, so having regular healthy meals and drinking plenty of fluids can give you more spare energy to reengage with your sex life.
Body Image
“Sexuality is not a concept that can be considered in separation from that of health; sexuality is in fact central to a person’s sense of wellness and self-concept”
– Sheppard & Ely, 2008 ⁸
Despite the lack of conversation about body image with regard to breast cancer and treatment, it remains a major symptom that can have a long-lasting impact. Any of the major changes to your body that we’ve mentioned so far can alter the way you think about yourself sexually. Viewing any negative self-perception as a legitimate symptom which can be managed and treated can help to make the process easier.
One key aspect that can affect body image is a change of weight during and following treatment. While many cancers are associated with chronic weight loss despite a normal diet, breast cancer is in fact more associated with chronic weight gain ⁹. Regardless of whether you’re putting on more or losing more weight than you’re used to, the change can serve as a constant reminder of your treatment and can knock your confidence. Speaking with your doctor about what aspect of treatment is causing the weight change is a good first step. Maggie’s has created a good resource for managing weight change during cancer which you can check out here.
Another issue that can affect body image is any scarring following breast cancer surgery. Beyond any of the pain or numbness that we have discussed previously, there can be a feeling of great loss in sexuality or femininity associated with a mastectomy or breast conserving surgery. It may also be difficult to come to terms with a new scar if you’re worried that a partner may see you differently. According to Sheppard & Ely ⁸, partners often wrongly assume their partners will be disturbed by the changes, so keeping an open dialogue with them about your feelings is bound to set some of those anxieties to rest.
Whatever aspect of your body that has been altered during treatment, the most effective tool for combatting a negative self-image is with self-compassion, the practice of actively being kind to yourself ¹⁰. While this may seem to be an obvious solution, it isn’t exactly obvious how to make this into a regular practice in our lives.
One exercise is to imagine that you’re speaking to a friend who has been through the same treatments and experiences you have and consider how you would treat them. You may find you have more patience with yourself. Additionally, how you treat yourself informs others around you how to treat you, so your positive feelings will be recognised by a partner.
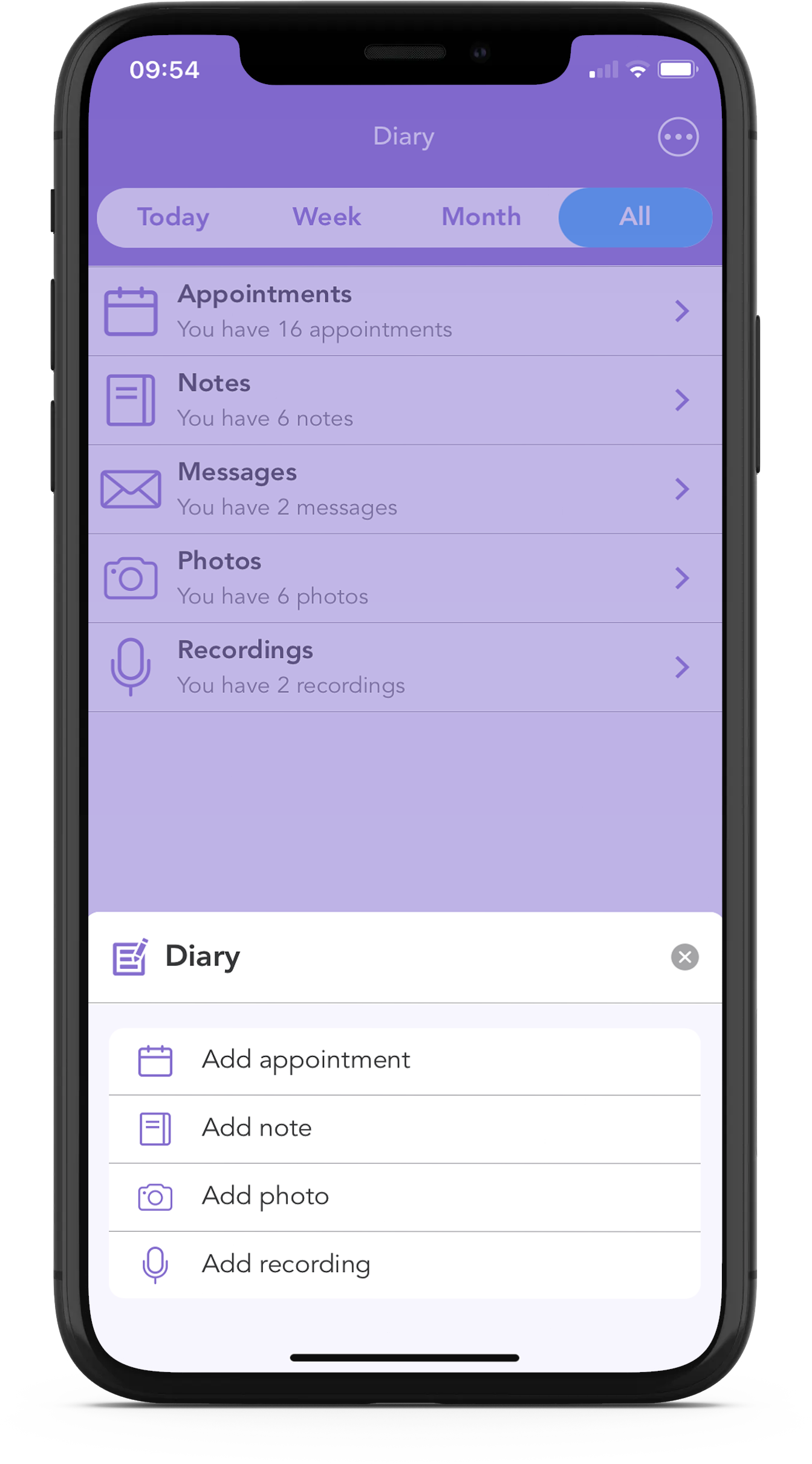
At OWise, one of our biggest goals is to help improve communication between you and your care team, and with the OWise breast cancer app, there are a number of tools to help with this. Using the Questions List feature, you can write down your sex and sexual health related questions so that you know exactly what you will ask before you arrive at the consultation. You can also make notes, store photos and audio-record your appointments, so that later on you can check if you missed something important.
The OWise app is big on security and privacy protection and what’s even better is that you can download it for free today!
Useful Links
Sex and Breast Cancer by Jo Divine
Is Your Lubricant Causing Thrush? by Jo Divine
Weight Changes and Cancer by Maggie’s
Pelvic Floor Exercises by NHS England
References
[1] Meyerowitz, B.E., Desmond, K.A., Rowland, J.H., Wyatt, G.E. and Ganz, P.A., 1999. Sexuality following breast cancer. Journal of Sex & Marital Therapy, 25(3), pp.237-250.
[2] Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M. and Sundquist, K., 2009. Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer nursing, 32(4), pp.271-280.
[3] Chatsiproios, D., Schmidts-Winkler, I.M., König, L., Masur, C. and Abels, C., 2019. Topical treatment of vaginal dryness with a non-hormonal cream in women undergoing breast cancer treatment-An open prospective multicenter study. PloS one, 14(1), p.e0210967.Younus, J. and Kligman, L., 2010.
[4] Younus, J. and Kligman, L., 2010. Management of aromatase inhibitor–induced arthralgia. Current Oncology, 17(1), p.87.
[5] Bower, J.E., 2014. Cancer-related fatigue—mechanisms, risk factors, and treatments. Nature reviews Clinical oncology, 11(10), p.597.
[6] Wilmoth, M.C., Coleman, E.A., Smith, S.C. and Davis, C., 2004, November. Fatigue, weight gain, and altered sexuality in patients with breast cancer: exploration of a symptom cluster. In Oncology nursing forum (Vol. 31, No. 6, pp. 1069-1080). 125 ENTERPRISE DR, PITTSBURGH, PA 15275 USA: ONCOLOGY NURSING SOCIETY.
[7] Barton-Burke, M., 2006. Cancer-Related Fatigue and Sleep Disturbances: Further research on the prevalence of these two symptoms in long-term cancer survivors can inform education, policy, and clinical practice. Cancer nursing, 29(2), pp.72-77.
[8] Sheppard, L.A. and Ely, S., 2008. Breast cancer and sexuality. The Breast Journal, 14(2), pp.176-181.
[9] Helms, R.L., O’Hea, E.L. and Corso, M., 2008. Body image issues in women with breast cancer. Psychology, Health and medicine, 13(3), pp.313-325.
[10] Przezdziecki, A., Sherman, K.A., Baillie, A., Taylor, A., Foley, E. and Stalgis‐Bilinski, K., 2013. My changed body: breast cancer, body image, distress and self‐compassion. Psycho‐oncology, 22(8), pp.1872-1879.
[11] Albers, L.F., van Belzen, M.A., van Batenburg, C., Engelen, V., Putter, H., Pelger, R.C. and Elzevier, H.W., 2020. Discussing sexuality in cancer care: towards personalized information for cancer patients and survivors. Supportive care in cancer, 28(9), pp.4227-4233.
