
Surgery is one of the first treatments a breast cancer patient receives. According to data from 2015, over 80% of people diagnosed with breast cancer in the UK had surgery and just under half (43%) of those had a mastectomy1. Mastectomy is an invasive surgical procedure where all the breast tissue is removed. This type of treatment for breast cancer is usually carried out due to:
- breast conserving surgery (lumpectomy) not being appropriate due to the size or characteristics of the tumour;
- personal reasons;
- having a very high risk of getting a second breast cancer, such as carrying the breast cancer susceptibility genes (BRCA1 or BRCA2) (to learn more about this, check out our BRCA blog).
The decision between a mastectomy and a breast conserving surgery
Previous studies have shown that breast cancer patients who chose to have either breast conserving surgery or mastectomy had a similar survival 2,3. Choosing a more invasive mastectomy surgery does not guarantee that you will live longer or that you will have less chance of cancer coming back 4,5.
“There’s so many things during this process that you have no control over, and then the biggest decision of the entire thing is kind of dropped in your lap and you’re like, no, I don’t feel like I should be making this decision.” (Crystal Collum, breast cancer patient, on her experience of choosing between surgery options)6
Recent data has shown that the rate of contralateral mastectomy (surgical removal of the opposite uninvolved breast) in women with early and unilateral breast cancer (tumour found only in one breast) is high and is increasing around the world7,8. Interestingly, a survey done in the United States found that women who were younger, Caucasian and more highly educated were more likely to opt for this procedure. However, they also found that the rate of this procedure was lower when their surgeon recommended against it9. This is just an example of how crucial patient communication is.
Did you know that the OWise app has a wide range of tools to improve communication with your doctors? The app offers you a list of suggested questions based on cancer’s characteristics for you to ask in the next consultation. Moreover, you can securely save audio recordings of your conversations with your care team, as well as sensitive photos, notes and treatments!
The types of Mastectomy available
A mastectomy is an aggressive surgical procedure that involves removing the entire breast tissue. There are four different types of mastectomy:
Total Mastectomy
The most common procedure is a total mastectomy with sentinel node biopsy, which has also been called a “Modified radical mastectomy”. In this procedure, the entire breast tissue along with a portion of the skin is removed.
The first lymph nodes that drain the breast tissue are called the sentinel nodes. These nodes are located in the armpit and are often removed through the same incision. These nodes may be evaluated by a pathologist while you are under anaesthesia and if they contain cancer, additional nodes can be removed during the surgical procedure.
A total mastectomy can also be done without a sentinel node biopsy when it is unnecessary to check the lymph nodes. This procedure is sometimes called a “Simple mastectomy”.
Skin Sparing Mastectomy
This is a surgery option for people with no cancer cells in the skin that want to have immediate breast reconstruction after the mastectomy. This procedure removes the entire breast, nipple and areola but leaves as much skin as possible to assist with reconstructing the breast by an oncoplastic surgeon (for more information about reconstruction, read below).
Nipple Sparing Mastectomy
A Nipple Sparing Mastectomy leaves the nipple, areola and skin intact. In this procedure, a small amount of tissue is left under the nipple to help maintain the blood supply. This surgery is an option for women with a small, early-stage tumour that is away from the nipple and have no cancer cells in the skin, nipple or lymph nodes below the armpit. It is usually followed by immediate reconstruction. This type of mastectomy can cause problems in the blood and nerve supply to the nipple, which may result in nipple discolouration and a lack of sensation. There is also a slightly higher risk of cancer recurrence in the skin left under the nipple. Ask your surgeon if you are a good candidate for this procedure.
An exciting project led by Prof Stacy Lindau is planned that will restore breast sensation loss and function after mastectomy by applying bionics. This could help breast cancer patients that lose sensation after a mastectomy with reconstruction or even after a lumpectomy! Their idea is to insert a flexible sensor under the skin. You can read more about it here.
Radical Mastectomy
A radical mastectomy removes all components of the breast, as well as the lymph nodes beneath the armpit and portions of the pectoralis major and minor muscles located in the chest wall. Although once very common, this surgical procedure is now not typically performed, except in some cases where cancer has invaded the chest wall muscle.
Did you know that in 1882, the first radical mastectomy was performed by William Halsted. Although now alternative surgeries are preferred, it was followed well into the 20th century with a ‘one-size’ fits all approach. Halsted’s procedure was revolutionary in the treatment of breast cancer, achieving a massively reduced local recurrence rate that had not been seen before at that time10.
What should I expect in a mastectomy?
- A mastectomy is usually performed under general anaesthesia. It can last from 2 to 3 hours and may involve one to three days of hospital recovery depending on the complexity of the procedure.
- Although incision details may vary depending on the type of mastectomy, usually a 6-8 inch (~15-20cm) elliptical incision around the nipple is performed and breast tissue is removed away from the overlying skin and underlying muscle. This is typically performed with an electrosurgery device that uses heat for cutting and minimises bleeding.
- If the breast is not being reconstructed immediately (see below), the incision will be closed with sutures or surgical staples.
- One or two temporary drains are often placed to remove any fluid that may accumulate after the surgery.
- To complete the procedure a dressing will be put over the incision.
Breast reconstruction
Breast reconstruction can be done at the same time as a mastectomy (immediate breast reconstruction) or at a later date (delayed breast reconstruction). For these types of procedures, a multidisciplinary breast cancer team is key as a surgical oncologist will be the one removing the tumour and the nearby tissue, and an oncoplastic surgeon will be the one performing the breast reconstruction.
You may also decide to have a mastectomy without reconstruction. If you want to maintain your former appearance, there are a variety of special bras, prostheses and breast forms that can be used under clothing.
Immediate reconstruction versus delayed reconstruction
Although breast reconstruction can be carried out either at the time of mastectomy (immediate) or at a later time (delayed), immediate reconstruction is usually the preferred option. Although some studies previously reported higher levels of patient well-being and satisfaction compared to delayed procedures11,12, recent studies suggest that delaying the reconstruction does not compromise the clinical outcome or the patients’ well-being and satisfaction13. Therefore, it is important that you and your care team discuss the advantages and disadvantages of each procedure. You can read more about the advantages and disadvantages of immediate versus delayed reconstruction here.
The types of breast reconstruction available
1. Implant breast reconstruction:
This usually involves the insertion of a prosthesis made of synthetic material. A typical implant is made of a silicone shell and is filled with saline or silicone gel. This is one of the simplest procedures and requires the shortest initial hospital stay. However, the response of the body to foreign material can result in the implant being squeezed by scar tissue leading to distorted shapes, ruptures and infections. Please discuss the possible adverse effects with your care team to help decide if this is the best option for you.
2. Natural tissue breast reconstruction (known as autologous or “flap” reconstruction):
This type uses the body’s own tissue for breast reconstruction. Tissue (skin, fat and even muscle) is usually taken from another part of your body and transferred to the chest to make a new breast. Possible donor tissue sites include the lower abdomen, buttocks, back and inner thighs, though the lower abdomen is usually the preferred area. This tissue allows the reconstruction of a breast that looks and feels more like a normal breast and solves the problem of the body’s immune system rejecting the implant. However, this type of reconstruction requires a longer hospital stay, additional scars and possible weakening of the donor site due to loss of muscle.
This type of reconstruction has evolved through the years, from TRAM flaps to DIEP and SIEA flaps. Read below to understand the advantages and disadvantages of each of them:
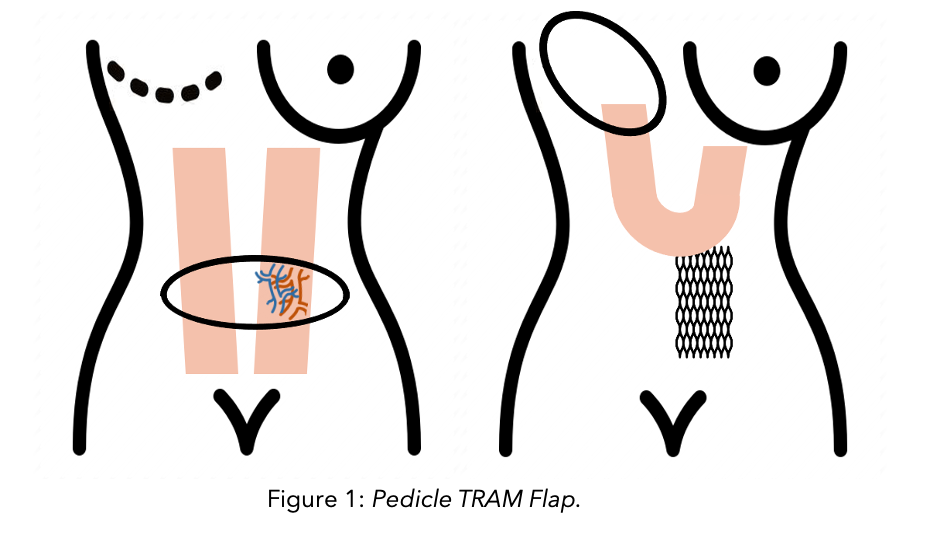
Pedicle TRAM (Transverse Rectus Abdominus Myocutaneous) Flap
A section of skin and fat (also called a flap) attached to the six-pack muscle in the abdomen is cut. This flap remains attached to the body by the six-pack muscle. It is then rotated and transferred to the new location in the chest. Here it is shaped to form the new breast and supplied by the blood vessels that support the muscle. A piece of synthetic mesh is placed in the abdomen to support the abdominal wall. The main disadvantage of this technique is the weakening of the abdominal wall as it requires a substantial loss of muscle.
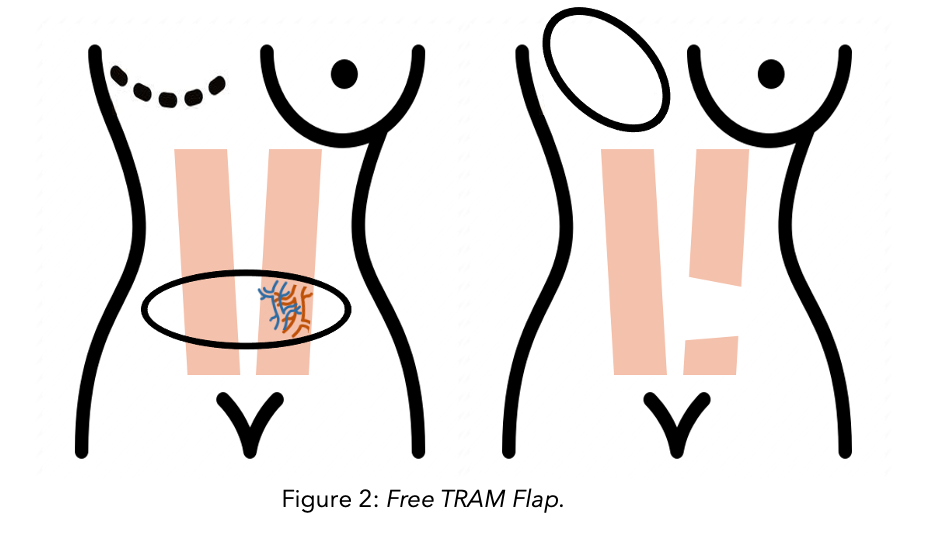
Free TRAM (Transverse Rectus Abdominus Myocutaneous) Flap
This is a developed and improved form of TRAM. For this, skin, fat, muscle and blood vessels from the lower abdomen are separated completely from the body and transferred to the breast. The blood vessels from the flap are called the deep inferior epigastric arteries and veins (see the diagram). These blood vessels are connected to the breast blood vessels by microsurgery techniques. With this technique, the blood supply to the breast is more robust and the flap is easier to sculpt into the desired shape. However, muscle loss is still significant, and it requires microsurgery expertise. Therefore, it might not be offered in your hospital.
DIEP (Deep Inferior Epigastric Perforator) Flap
In this procedure, skin, fat and blood vessels are taken from the lower abdomen but no muscle is removed. Similarly, to the free TRAM, the blood vessels taken from the abdomen are the deep inferior epigastric artery and vein, which are then connected to the breast blood vessels by microsurgery techniques. The main advantage is that since no muscle is taken, the abdominal wall is not weakened.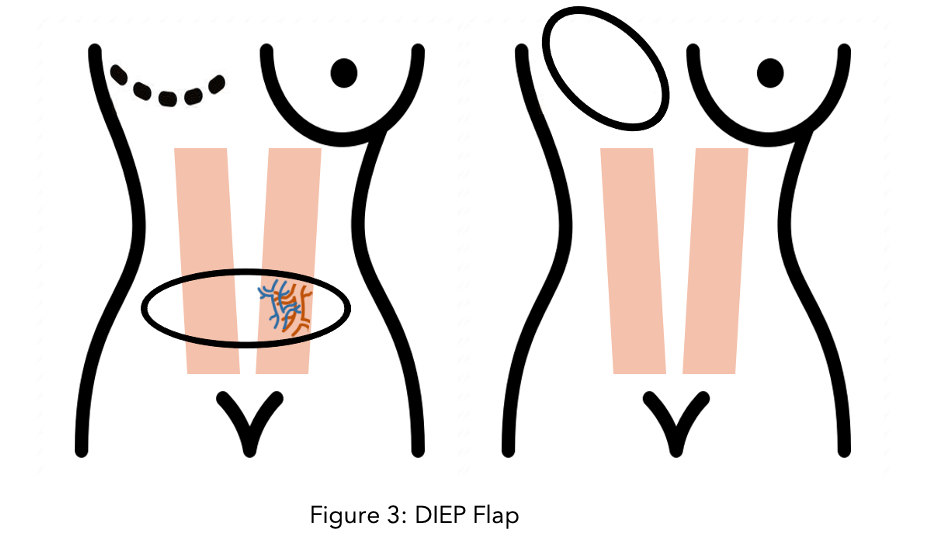
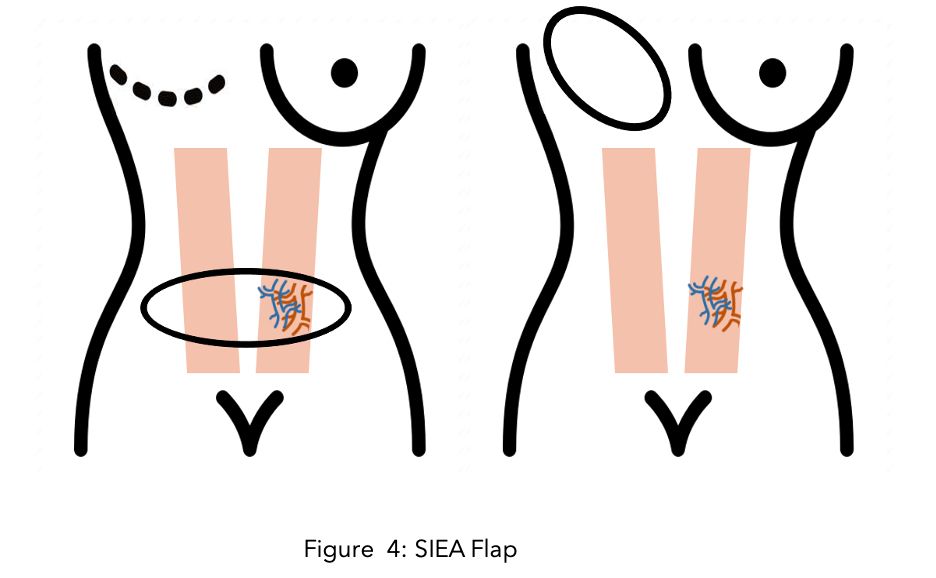
SIEA (Superficial Inferior Epigastric Artery and Vein) Flap
This is a similar procedure to DIEP, but the blood vessels that are taken from the abdomen are superficial inferior epigastric arteries and veins (see the diagram). These vessels run in the fat layer so with this procedure the abdominal wall is left untouched. Although this is the preferred method whenever possible, the reason why this is not widely used is because these vessels are not large enough in 90% of patients.
For more information about breast reconstruction, the Breast Advocate app includes a wide range of articles and resources to understand the different reconstructive options. You can also find pictures of different breast reconstructions here.
Side effects
Patients are usually amazed at the speed of the recovery and severe or prolonged pain after surgery is rare. The most common side effects are:
 Numbness beneath the incision or in the armpit and a temporary burning sensation in the upper inner arm if nodes have been removed.
Numbness beneath the incision or in the armpit and a temporary burning sensation in the upper inner arm if nodes have been removed. - A seroma which is a build-up of fluid under the arm.
- The weakening of the abdominal wall.
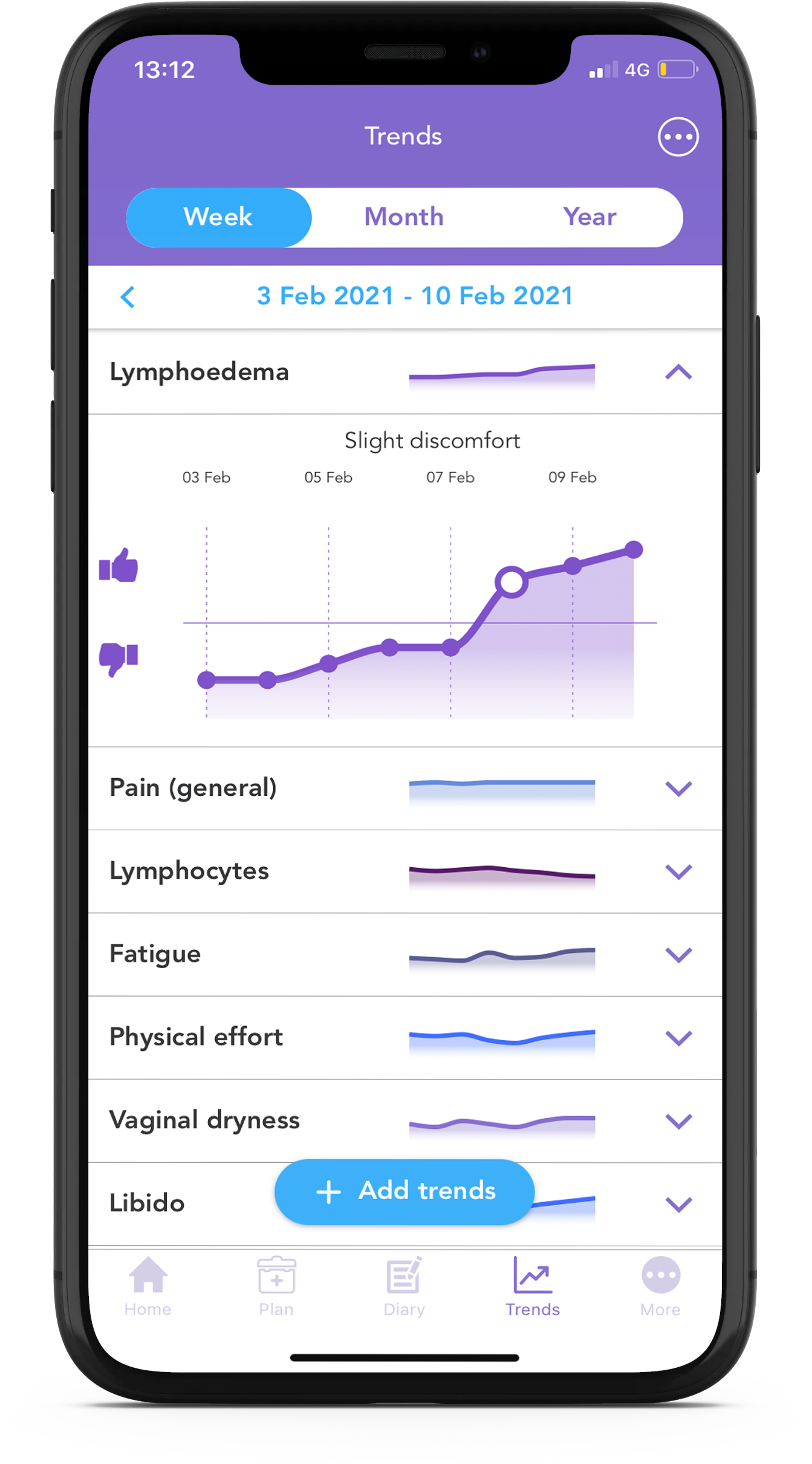
- Lymphoedema and cording:
- Lymphoedema is a build-up of fluid in the arm that causes swelling, pain and tenderness in your arm and hand.
- Cording, also known as axillary web syndrome (AWS) is a condition in which a rope-like soft-tissue density develops in the axilla. The cords tend to be painful and tight, making it difficult for you to lift your arm any higher than your shoulder or extend the elbow fully.
Read our Lymphoedema and Cording blog to learn more about how these conditions develop and management strategies.
We hope you enjoyed reading our blog and that with this knowledge, you better understand the different mastectomy and breast reconstruction options. Our aim is to make sure you are always kept informed. Follow our Instagram and Facebook accounts for any updates including the next blog of this surgery miniseries.
To receive more personalised information regarding your type of breast cancer, download the OWise app today from the iOS App Store or Google Play Store.
References
- Breast Cancer Care. 2015. Breast Cancer Numbers... [online]. Available at: https://breastcancernow.org/sites/default/files/files/breast-cancer-stats-sheet-february-2015.pdf[Accessed February 2021].
- Lichter, AS., Lippman, ME., Danforth, DN., d’Angelo, T., Steinberg, SM., deMoss, E., MacDonald, HD., Reichert, CM., Merino, M., Swain, SM. 1992. Mastectomy versus breast-conserving therapy in the treatment of stage I and II carcinoma of the breast: a randomized trial at the National Cancer Institute. J Clin Oncol. 10(6), pp:976-983.
- Riedel, F., Hennings, A., Hug, S., Schaefgen, B., Sohn, C., Schuetz, F., Golatta, M., Heil, J. 2017. Is Mastectomy Oncologically Safer than Breast Conserving Treatment in Early Breast Cancer. Breast Care. 12, pp: 385-390.
- Quan, G., Pommier, SJ., Pommier, RF. 2008. Incidence and outcomes of contralateral breast cancers. Am J Surgery. 195(5), pp: 645:650
- Lostumbo, L., Carbine, NE., Wallace, J., Ezzo, J., Dickersin, K. 2004. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev.4
- Caruso, C. Why a growing number of women with breast cancer are choosing double mastectomy. 2017. Health. [online]. Available at: https://www.statnews.com/2017/08/29/double-mastectomy-breast-cancer
- Wong, SM, Freedman, RA., Sagara, Y., Aydogan, F., Barry, WT., Golsham, M. 2017. Growing use of contralateral prophylactic mastectomy despite no improvement in long‐term survival for invasive breast cancer. Ann Surg.265(3), pp: 581-589.
- Yao, K., Winchester, DJ., Czechura, T., Huo D. 2013. Contralateral prophylactic mastectomy and survival: report from the National Cancer Data Base, 1998–2002. Breast Cancer Res Treat.142(3), pp: 3465-3476.
- Jagsi, R., Hawley, ST., Griffith, KA., Janz, NK., Kurian, AW., Ward, KC., Hamilton, AS., Morrow, M., Katz, S. 2017. Contralateral Prophylactic Mastectomy Decisions in a Population-Based Sample of Patients With Early-Stage Breast Cancer. JAMA Surg ;152(3), pp:274–282.
- Mukherjee Siddhartha. 2010. The emperor of All Maladies. Scribner
- Wellisch, DK., Schain, WS., Noone, RB., Little, JW. 1985. 3rd Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg. 76(5), pp: 713–
- Yoon, AP., Qi, J., Brown, D., Kim, HM., Hamil, JB., Erdmann-Sager, J., Pusiz, AL., Wilkins, EG. 2017. Outcomes of immediate versus delayed breast reconstruction: Results of a multicenter perspective study. Breast. 37; pp: 73-79.
- Al-Ghazal, SK., Sully, L., Fallowfield, L., Blamey, RW. 2000. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 26(1), pp: 17–9.
