 Peripheral neuropathy is when nerve damage leads to symptoms such as tingling, numbness and pain in the hands and feet. In some cases, chemotherapy can cause this condition, known as chemotherapy-induced peripheral neuropathy (CIPN). Chemotherapy drugs target fast-growing cells in the body, such as cancer cells, but they can also harm normal fast-growing cells like those in the nervous system. As a result, CIPN can pose challenges with daily activities such as getting dressed, balance and cooking1. This blog will help you better understand what CIPN is, how it arises and strategies to manage it.
Peripheral neuropathy is when nerve damage leads to symptoms such as tingling, numbness and pain in the hands and feet. In some cases, chemotherapy can cause this condition, known as chemotherapy-induced peripheral neuropathy (CIPN). Chemotherapy drugs target fast-growing cells in the body, such as cancer cells, but they can also harm normal fast-growing cells like those in the nervous system. As a result, CIPN can pose challenges with daily activities such as getting dressed, balance and cooking1. This blog will help you better understand what CIPN is, how it arises and strategies to manage it.
What is chemotherapy-induced peripheral neuropathy (CIPN)?
According to The National Cancer Institute, CIPN is a condition characterised by nerve damage that can cause uncomfortable sensations like pain, numbness, tingling, swelling, or muscle weakness in different parts of the body2. CIPN happens when the nerves outside of the brain and spinal cord, called the peripheral nerves, are damaged by chemotherapy drugs. These peripheral nerves are like messengers that transfer signals from the brain to other parts of the body. This allows the feeling of sensations and ability to control the movement of muscles around the body.
Where CIPN is experienced in the body depends on which nerves are affected and the chemotherapy drugs involved. Usually, it happens in the hands and feet, but it can also happen in other areas such as the arms, legs and even the face. Research shows that there is still a large amount of people that experience symptoms of CIPN late after chemotherapy3:
- 68% after 1 month of chemotherapy
- 60% after 3 months of chemotherapy
- 30% after 9 months of chemotherapy
How does chemotherapy cause peripheral neuropathy?
Taxane chemotherapy, like docetaxel (Taxotere®) and paclitaxel (Taxol®), are treatments for breast cancer4. Neuropathy is one of the most common side effects caused by taxanes, but why exactly does this happen?
In the body, taxanes interact with a protein on the outside of a certain type of white blood cell (macrophages). These macrophages are a part of the immune system, which works to protect us. When immune cells get activated, this triggers events that cause inflammation and stress in nerve cells. This stress reduces the energy produced and stored in cells, causing damage and affecting their ability to work properly. Thereby, chemotherapy drugs can cause a series of events that can lead to inflammation and stress in nerve cells, potentially resulting in nerve damage and CIPN symptoms5.
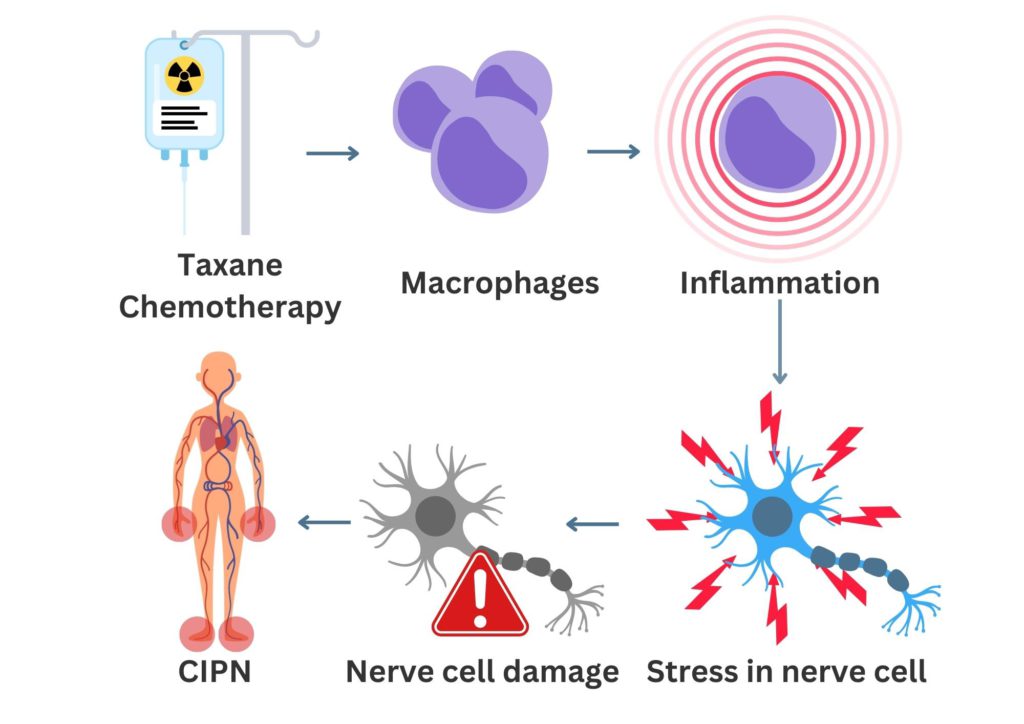
Figure 1. Taxane chemotherapy causing the inflammation of macrophages. This leads to the stress of nerve cells resulting in damage, which can cause symptoms of CIPN.
What increases the risk of developing peripheral neuropathy?
Peripheral neuropathy can be caused by different types of chemotherapy drugs. The likelihood of developing peripheral neuropathy increases with multiple treatment courses, use of combination chemotherapy and higher doses. Peripheral neuropathy can also be caused by other things besides chemotherapy, such as surgery, radiation therapy, physical injury, infections affecting the nerves and some autoimmune disorders. Other risk factors include6,7:
- Age
- Diabetes
- Vitamin deficiencies (e.g. low vitamin B levels)
- Alcohol abuse
If you would like to learn more about how to navigate chemotherapy safely, head over to the blog ‘Chemotherapy and Breast Cancer: Navigating Treatment Safely‘.
What are the symptoms of peripheral neuropathy?
A large study performed in The Netherlands looked at the experiences of cancer survivors with peripheral neuropathy. They made an overview of common symptoms, daily limitations, involvement of healthcare professionals, and social support. The most common symptoms were tingling and loss of sensation or diminished sensation. Daily tasks like household chores, hobbies, walking and sleeping were where people struggled the most8.
Most commonly symptoms are noticed in the hands and feet, these can include:
- Decreased sensation or numbness
- Muscle weakness
- Tingling (pins and needles)
- Discomfort or pain
- Increased sensitivity to touch, temperature, pain and pressure
Symptoms of CIPN can vary depending on which peripheral nerves are affected. There are three different types of peripheral nerves: autonomic, sensory and motor nerves. See below specific symptoms related to the different types of nerve damage9.
Sensory nerves carry signals to your brain to help you process information from your environment via touch, vision taste and smell. Damaged sensory nerves can lead to:
- Numbness, tingling
- Inability to feel pain
- Inability to feel hot or cold
Motor nerves are responsible for the movement of your muscles. Damaged motor nerves can lead to:
- Muscle weakness. This could cause potential balancing issues, easy stumbling, or challenges in tasks like opening a jar
- Cramps or twitching of your muscles
Autonomic nerves control things like blood pressure, heart rate, temperature, digestion, and urination. The symptoms of autonomic nerves may be more subtle and harder to identify as they can be influenced by a lot of different factors. Symptoms can include:
- Dizzy or faint feeling because of low blood pressure
- Digestive changes
- Sexual difficulties (men may be unable to get an erection and women to reach an orgasm)
- Sweating problems
- Urination problems
The duration and severity of these symptoms can differ from person to person. Some may have more noticeable issues related to sensory and motor nerves, while symptoms of autonomic nerve damage may be less obvious. If you start noticing any of the symptoms listed above, it is important to talk to your doctor or nurse. Finding and treating these problems early is the best way to manage them.
Do you know that you can track your side effects with OWise? With more than 30 side effects and symptoms to choose from, you can track any changes and share these with your care team and loved ones via a secure hyperlink. Having a better communication with your care team can make sure you receive the best care possible.
Managing peripheral neuropathy, what can I do?
At this moment, there is not an effective way to prevent peripheral neuropathy1. However, there are steps you can take to manage your symptoms. When you are experiencing symptoms, your doctor might decide to pause your treatment or lower the chemotherapy dose until your symptoms improve. It is important to act as soon as your symptoms start to prevent any lasting damage.
Symptoms can be present temporarily or for a longer amount of time, for which you might need ongoing treatment. The main goal of treatment for peripheral neuropathy is generally to alleviate pain. These are some examples of pain medicine:
- Numbing medicine patches or creams. This can be applied directly on the painful area, such as lidocaine patches or capsaicin cream.
- Steroids. These may be used for short-term until a long-term plan is made.
- Anti-seizure medicine. These are known for their effectiveness in managing various forms of nerve pain.
- Antidepressant medications. Typically used in smaller doses than those used for depression treatment.
- Opioids or narcotics. They are only prescribed for severe pain.
Finding the right solution might require some trial and error to determine what works best for you.
Managing peripheral neuropathy symptoms9,10:
- Try to prevent falls. Ask someone to help you move away objects that increase the risk of tripping, like rugs. Take your time when getting up after sitting or lying down, especially if you feel dizzy.
- Give yourself more time to do things. Remind yourself that it is okay to take a bit longer. And ask friends or family to help you with difficult tasks.
- Try to stop or limit drinking alcohol. Drinking alcohol can lead to nerve damage and might make your symptoms worse.
- For people with diabetes, it is crucial to manage your blood sugar levels. Elevated blood sugar levels can potentially lead to nerve damage.
- Stay active and consider incorporating regular exercises to improve your balance and coordination. Physical activity has been shown to be a valuable therapeutic approach, with the potential of alleviating neuropathic pain over time11. Recent research showed that performing a specific type of exercise called ‘sensorimotor training’ at least two times a week, is especially beneficial for people with peripheral neuropathy caused by chemotherapy12. This specialized training focuses on improving coordination and communication between the nervous system and the muscles and joints. It includes exercises that train your balance and coordination. For an exercise programme tailored to your needs, we advise you to consult a physical or occupational therapist.
- Ask about pain medicine or integrative medicine practices. In the previous section we described some examples of pain medicine. Next to this, alternative methods such as massage, acupuncture, and yoga may be recommended at times to alleviate pain.
- Talk to your healthcare team. Ask them questions like: what symptoms do I need to watch out for? What precautions should I take to stay safe? Or: could you direct me to a specialist who can provide extra guidance?
You could be more prone to accidentally hurting yourself when your sense of feeling is affected. These are some tips to avoid injury:
- Protect from heat injuries. Lower the temperature of your hot water heater to minimize the risk of scalding. Make sure to use oven gloves when dealing with hot dishes or pans.
- Protect your hands. When you do work outdoors or clean, use gloves for protection.
- Avoid extreme temperatures. Make sure to keep your hand and feet warm and covered during wintertime.
- Wear sturdy shoes that cover your whole foot. Wear shoes both inside and outside. You could ask your healthcare team about special shoes or inserts to help protect your feet.
- Support yourself when walking. If you have problems with stumbling while walking, you could use a walker or cane to get extra support. Think about installing rails on walls and in the bathroom to provide a steady grip for balance.
Research showed that support from professionals, family and friends is very important in managing peripheral neuropathy8. Social support can alleviate various aspects of disease such as coping with stress, anxiety, depression, and quality of life13. It has been highlighted that patients who received medium to high levels of social support experienced less severe symptoms compared to people with low levels of support14. Don’t forget to remind yourself or your loved-one that it is very important to talk about how you feel to people in your environment. You could also consider inquiring about dedicated support groups for people who share similar experiences.
And that’s chemotherapy-induced peripheral neuropathy summed up
We hope that this blog helped you understand how chemotherapy can lead to peripheral neuropathy, how to recognize symptoms and what to do to manage it. As you are dealing with symptoms, always remember that you are not alone. Whether you are experiencing peripheral neuropathy yourself or helping a loved one through it, the importance of social support cannot be overstated. Don’t hesitate to share your experiences with the people around you and ask for extra support when needed.
This blog is the third in our chemotherapy series, where we will cover different side-effects, patient experiences and the latest developments in the field. So, stay tuned for the upcoming blog posts. At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Facebook for any updates. Any questions? Get in touch!
References
- Zajączkowska R, Kocot-Kępska M, Leppert W, Wrzosek A, Mika J, Wordliczek J. Mechanisms of Chemotherapy-Induced Peripheral Neuropathy. International Journal of Molecular Sciences. 2019;20(6):1451.
- Institute NC. NCI Dictionary of Cancer Terms: neuropathy [Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/neuropathy.
- Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, Macleod MR, et al. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: A systematic review and meta-analysis. Pain. 2014;155(12):2461-70.
- Tkaczuk K, Yared J. Update on taxane development: new analogs and new formulations. Drug Design, Development and Therapy. 2012:371.
- Burgess J, Ferdousi M, Gosal D, Boon C, Matsumoto K, Marshall A, et al. Chemotherapy-Induced Peripheral Neuropathy: Epidemiology, Pathomechanisms and Treatment. Oncology and Therapy. 2021;9(2):385-450.
- Brown TJ, Sedhom R, Gupta A. Chemotherapy-Induced Peripheral Neuropathy. JAMA Oncology. 2019;5(5):750-.
- team TACSmae. What Is Peripheral Neuropathy? 2019 [Available from: https://www.cancer.org/cancer/managing-cancer/side-effects/nervous-system/peripheral-neuropathy/what-is-peripherial-neuropathy.html.
- Van De Graaf DL, Engelen V, De Boer A, Vreugdenhil G, Smeets T, Van Der Lee ML, et al. Experiences of cancer survivors with chemotherapy-induced peripheral neuropathy in the Netherlands: symptoms, daily limitations, involvement of healthcare professionals, and social support. Journal of Cancer Survivorship. 2023.
- Institute NC. Nerve Problems (Peripheral Neuropathy) and Cancer Treatment 2020 [Available from: https://www.cancer.gov/about-cancer/treatment/side-effects/nerve-problems.
- team TACSmae. Managing Peripheral Neuropathy 2021 [Available from: https://www.cancer.org/cancer/managing-cancer/side-effects/nervous-system/peripheral-neuropathy/managing-peripheral-neuropathy.html.
- Wonders KY, Whisler G, Loy H, Holt B, Bohachek K, Wise R. Ten Weeks of Home-Based Exercise Attenuates Symptoms of Chemotherapy-Induced Peripheral Neuropathy in Breast Cancer Patients. Health Psychol Res. 2013;1(3):e28.
- Streckmann F, Balke M, Cavaletti G, Toscanelli A, Bloch W, Décard BF, et al. Exercise and Neuropathy: Systematic Review with Meta-Analysis. Sports Medicine. 2022;52(5):1043-65.
- Parker PA, Baile WF, Moor CD, Cohen L. Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psycho-Oncology. 2003;12(2):183-93.
- Oh GH, Yeom CW, Shim EJ, Jung D, Lee KM, Son KL, et al. The effect of perceived social support on chemotherapy-related symptoms in patients with breast cancer: A prospective observational study. J Psychosom Res. 2020;130:109911.
