 This blog was written by Naman Julka-Anderson and Jo McNamara, the founders of Rad Chat. Be sure to check out their podcast and follow them on instagram for all things radiotherapy and oncology.
This blog was written by Naman Julka-Anderson and Jo McNamara, the founders of Rad Chat. Be sure to check out their podcast and follow them on instagram for all things radiotherapy and oncology.
What is radiotherapy?
Radiotherapy (RT) is a type of radiation treatment delivered typically with a Linear Accelerator (LA) (image 1), it is also sometimes referred to as External Beam Radiotherapy (EBRT). Radiotherapy is the use of very high ionising radiation (X-rays) that are manipulated to target cancer cells.

1 in 4 people in the UK will need radiotherapy at some point in their lives and radiotherapy is responsible for 40% of cancer cures1. It is often used alongside other treatments such as surgery, chemotherapy, immunotherapy and hormone therapy. Radiotherapy can be utilised with a curative intent, or it may be used to help improve quality of life of those receiving supportive and palliative care2.
Postoperative radiotherapy remains an integral part of breast-conserving therapy, providing remarkably consistent local control and overall survival. You may have radiotherapy to the entire breast area, or just to the area where the tumour started, this is known as partial breast radiotherapy. You may also have your lymph nodes irradiated to ensure that any remaining cancer cells are destroyed. Radiotherapy is sometimes referred to as the ‘insurance policy’ following surgery and/or chemotherapy. If you have a very low risk of the cancer returning after surgery you may not be offered radiotherapy3.
How does radiotherapy for breast cancer work?
Radiotherapy does not distinguish between normal healthy cells and cancer cells; the difference is that our normal healthy cells have the capacity to repair and repopulate. Everyone who receives radiotherapy has a very personalised radiotherapy treatment plan which is created from a pre-treatment CT scan. The radiotherapy treatment plan is created to minimise the dose to normal healthy cells and maximise the dose administered to the cancer cells, or where the cancer cells may have been, if you have had previous surgery and/or chemotherapy. Radiotherapy is usually started between 4-8 weeks post-surgery or chemotherapy. However, there are waiting times and this can be longer, please do discuss this with your oncologist if you are at all concerned4.
How is radiotherapy given for breast cancer?
Radiotherapy is prescribed as a dose of radiation (Gy), over a number of days (known as fractions, often displayed as #). The dose and fractionation prescribed is personalised and can vary depending on your diagnosis, the area being treated, stage of cancer, grade of cancer and your overall health. Until recently it was standard practice for people with invasive breast cancer having surgery to have 40Gy over 15 fractions (3 weeks). The updated guidelines recommend that people should be offered 26Gy in 5 fractions (1 week) as part of routine practice. Some people can still be offered a higher dose and intensity of radiotherapy if they have a diagnosis that increases sensitivity to radiotherapy, or have had implant–based reconstruction, or have any other factor (such as a high BMI) that could mean having radiotherapy over 3 weeks is more acceptable5,6.
Did you know that you can add your radiotherapy treatment plan on the OWise app? Simply go to ‘Plan’, select radiotherapy treatment and choose how many fractions you have been prescribed. You can select your treatment start and end date then visualise your treatment plan as a chart or list.
Radiotherapy is typically administered every single day, except for the weekends. The radiotherapy department is not open to all patients on a weekend, as it is reserved for emergency cases only and allows for the radiotherapy engineers, the dosimetrists and physicists to undertake work ensuring the maintenance of the software and equipment, whilst also working on radiotherapy treatment plans and undertaking research.
Breast cancer radiotherapy pre-treatment CT scan

The radiotherapy pathway typically starts with a pre treatment appointment. This will involve a pre-treatment scan. This is similar to a diagnostic CT scan, however, we are not looking to use this scan in a diagnostic way, but more as a tool to plan your radiotherapy treatment. When you attend for the pre-treatment CT scan (Image 2) the therapeutic radiographers will talk you through the procedures and your consent. Please do utilise this time to talk through any concerns, or questions you may have.
For your appointment you may be asked to wear a gown, or remove all clothes from above the waist. The pre-treatment CT room can be cold, as the machine requires a cool environment to operate. Therefore, you may wish to consider wearing a hat and some gloves. Please be aware that although we may need to expose the area where we will be treating we will try to maintain your dignity and respect at all times.
Radiotherapy position
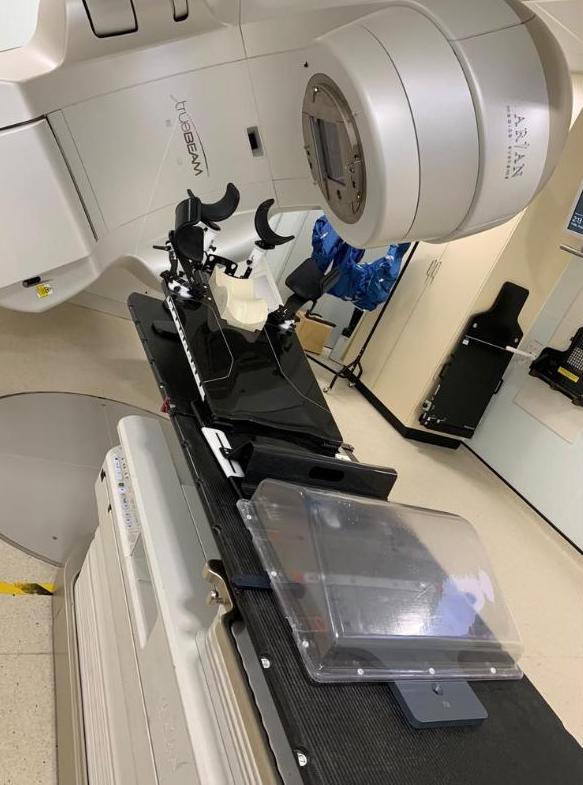
Within each department the technique used to deliver the radiotherapy may be slightly different because of variations in equipment and software. Irrespective of that, you will likely be placed on a piece of equipment called a breast board (Image 3). This is a slightly inclined board, with a neck and head support, a lower back support and arm supports to position your arms above your head. This is the position we will need you to be in for treatment, so getting yourself comfortable and relaxed is imperative at this stage.
It is advisable to practice this position after your surgery as much as possible and maintain the physiotherapy exercises your received to ensure it is a comfortable position that you can maintain for 20 minutes or so. You will see there are some laser lights shone onto your skins surface and these will be marked with pen. Again, please do ensure you are in a comfortable position and are as relaxed as possible, if you don’t feel comfortable then let the therapeutic radiographers know, there are lots of things they can do to try and make you more comfortable. If you are anxious, consider bringing along some music to listen to. You may be in this position for about 15 minutes and so making sure you can maintain this position comfortably is important.

When you are in the correct position the radiographers will then leave the room to conduct the CT scan. You will feel the couch move in and out of the CT scanner, you won’t see or feel anything and you will just hear a whirring noise. The therapeutic radiographers will then come back into the room and give you some permanent tattoos where the laser lights align, these tattoos are very small and are typically the size of a freckle. These tattoos will ensure that when you come to have radiotherapy treatment on a daily basis you can be aligned correctly in exactly the same position as you were for your CT scan.
If your department has Surface Guided Radiotherapy (SGRT) equipment8 and/or employs a technique called Deep Inspiration Breath Hold used for left sided breast and chest wall treatment, your pre-treatment CT scan may be slightly different. This resource is brilliant in helping you to prepare for this technique9. The CT scan and all the data is used to create a radiotherapy treatment plan. This planning process is complex and can take around 2 weeks or so, hence a few weeks gap between your planning pre-treatment appointment and the start of treatment.
Tips to help prepare for breast cancer radiotherapy treatment
Here is some simple advice to help you prepare for radiotherapy treatment, we will delve into this in more detail in a future blog:
- Let your therapeutic radiographers know if you have a time preference for your radiotherapy treatment
- Stop/reduce smoking
- Stop/reduce alcohol consumption
- Review your nutrition, you may consider increasing protein intake and eating more fresh fruit and vegetables.
- Increase your physical activity
- Keep practicing your radiotherapy position and continuing your physiotherapy exercises
- Moisturise your skin to improve the condition of your skin ahead of treatment. Review the skincare guidelines10
Getting radiotherapy treatment for breast cancer
When you arrive on your first day you will typically meet a therapeutic radiographer who will talk you through the treatment, reiterate consent and go through the short term side effects of treatment. You may be asked to get changed into a hospital gown, or you may prefer to wear something you can quickly and easily remove in the treatment room.
When in the radiotherapy treatment room you will be asked to lie in the same position you were in for your pre-treatment CT scan. The therapeutic radiographers will align your tattoos with the laser lights and at this point all you need to do is lie nice and still and breathe away normally (unless you are using the DIBH technique). The radiographers may need to move you slightly to help align the tattoos to the laser lights, sometimes this is just millimetres so please do not try to help us. When we have replicated your position, we need you to lie as still as possible and breathe away normally. The therapeutic radiographers will have to leave the room to deliver the radiotherapy, on their way out you may hear a loud buzzing noise, this is just an alarm we use to ensure no person is left in the room.
When outside the room therapeutic radiographers will be watching you the entire time on the TV screens and they may talk to you on the intercom. You will not feel anything, but you will hear whirring and clicking. The linear accelerator moves around you and should not touch you at any point, although it does come very close. The treatment will take 10 minutes or so. If your radiotherapy department uses surface guided radiotherapy, and/or deep inspiration breath hold techniques there may be slight differences in your radiotherapy treatment set up.
And that is radiotherapy for breast cancer summed up
This blog is the first blog in a radiotherapy series written by Rad Chat, where they will cover how to prepare for radiotherapy treatment, side effects of radiotherapy and radiotherapy for secondary (metastatic) breast cancer. So, stay tuned for the upcoming blog posts.
At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Twitter for any updates. Any questions? Get in touch!
References
- Radiotherapy UK https://radiotherapy.org.uk/get-involved/r4l-campaign-page/key-facts/#:~:text=Radiotherapy%20is%20needed%20in%2050,times%20more%20effective%20than%20chemotherapy(Accessed 19.1.24)
- Jacobson G, Kaidar-Person O, Haisraely O, Galper S, Rabin T, Dromi Shahadi I, Lawrence YR, Symon Z, Akiva Ben-David M. Palliative radiation therapy for symptomatic advance breast cancer. Sci Rep. 2021 Mar 5;11(1):5282. doi: 10.1038/s41598-021-84872-9. PMID: 33674709; PMCID: PMC7970854.
- Royal College of Radiologists. Radiotherapy dose fractionation, third edition – breast cancer https://www.rcr.ac.uk/media/h35isz40/rcr-publications-radiotherapy-dose-fractionation-third-edition-03-breast-cancer-march-2019.pdf (Accessed 20.1.24)
- Cancer Research UK https://www.cancerresearchuk.org/about-cancer/treatment/radiotherapy/external/what (Accessed 19.1.24)
- National Institute for Health and Care Excellence. 2022 exceptional surveillance of early and locally advanced breast cancer: diagnosis and management (NICE guideline NG101) https://www.nice.org.uk/guidance/ng101/resources/2022-exceptional-surveillance-of-early-and-locally-advanced-breast-cancer-diagnosis-and-management-nice-guideline-ng101-pdf-14432616076741 (Accessed 19.1.24)
- Ajithkumar, Thankamma, ‘Principles of radiotherapy’, Radiotherapy Planning, Oxford Specialist Handbooks in Oncology (Oxford, 2023; online edn, Oxford Academic, 1 Mar. 2023),https://doi.org/10.1093/med/9780198722694.003.0001, (Accessed 19.1.24)
- Liz O’Riordan Blog https://liz.oriordan.co.uk/2016/03/13/just-radiotherapy-to-go/ (Accessed 19.1.24)
- VisionRT https://www.visionrt.com/technology/sgrt/ (Accessed 20.1.24)
- Respire https://www.respire.org.uk/about (Accessed 19.1.24)
