This blog was written by Naman Julka-Anderson and Jo McNamara, the founders of Rad Chat. Be sure to check out their podcast and follow them on instagram for all things radiotherapy and oncology.
Preparing for radiotherapy for Breast Cancer
Rad Chat always advises patients to talk to their oncologist and therapeutic radiographers about their individual radiotherapy treatment as radiotherapy is very personalised. The information we have provided is very generalised, but should help you consider how to prepare and the questions to ask your team.
Please try not to compare your radiotherapy regime to others. Your oncologist, or consultant therapeutic radiographer will prescribe the best radiotherapy dose and fractionation for you. Some patients may just receive five treatments and others may receive many more, this is dependent on lots of factors and the department’s radiotherapy protocol. Please ask for clarification when being consented for radiotherapy(10).
Starting your treatment in the best possible health will lessen your side effects and help you cope emotionally and physically with the demands of cancer treatment. This blog will help you prepare and covers general advice, mental health support, mobility, radiotherapy techniques, radiotherapy appointments, understanding your radiotherapy treatment plan, skincare, managing fatigue and listening to your body.
General advice to prepare for radiotherapy for Breast Cancer
Our biggest piece of advice would be to start making healthy lifestyle choices as soon as you can. We call this ‘behaviour change’ and it can take up to 10 weeks for habits to form(1), so starting as soon as you have a diagnosis can be beneficial. You can do this by:
- Stopping smoking: If you smoke, seek support for smoking cessation ASAP. Your radiotherapy side effects (such as skin reactions) are likely to be more severe if you smoke through treatment(1,2).
- Reducing alcohol intake: Start to omit alcohol where you can as it dehydrates you and can increase symptoms of fatigue(2). There is support available for patients who depend on alcohol and need help to quit drinking, this will in turn improve your overall health, as well as lessen your side effects.
- Increasing fluid intake: Radiotherapy does cause cellular damage and so increasing your fluid intake will help with repair and growth, as well as excretion. Everyone is different and so your fluid intake should be personalised. However NHS guidance is 6-8 glasses of fluid a day, so also try to ditch the tea and coffee which are diuretics and will therefore make you urinate more and can actually dehydrate you. Switch to the water instead if you can. Maintaining hydration can also help with the symptoms of fatigue.
- Improving diet: Start to make positive changes to your diet, lots of fruit and vegetables, fibre and protein. This will help with cellular repair and also assist with fatigue(3). People having cancer treatment should try and consume more protein. You may need 1.0-1.5g per kg body weight, again this is something to discuss with your oncology team and specifically a dietitian if you have access to one.
- Engaging in physical activity: Move your body as you can, walk to the local shop, rather than drive, go for a walk rather than watching the TV. Being out in fresh air and getting some exercise is beneficial for your physical and mental health and can also boost your energy(4). If you have mobility issues or have a disability that may affect your ability to increase your physical activity it is always best to seek support from a physiotherapist.
Mental health support for radiotherapy for Breast Cancer
Cancer affects everyone differently, but some of the feelings people say they feel is anger, guilt, frustration, hopelessness, anxiety, isolation and sadness. It is really important to acknowledge what you’re going through is difficult, both emotionally and physically. Your oncology team should help you try and find a new normal, however, this may come after all your treatment has finished.
Radiotherapy, even when being used to cure your cancer, can leave you with lasting consequences. The late effects of treatment are very personalised and varies from person to person. Late effects can arise from 6 months to 20+ years post-treatment. Starting to process this and adapt physically to your new body can be challenging and be open to accessing support and advice for your mental wellbeing. If you have an existing mental health problem, you might find it harder to cope during this time. Reach out to your GP early on, so that support can be put in place, sooner, rather than later.
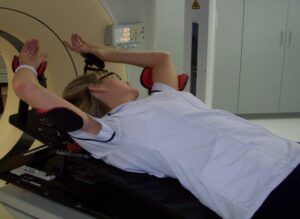
Mobility and radiotherapy for Breast Cancer
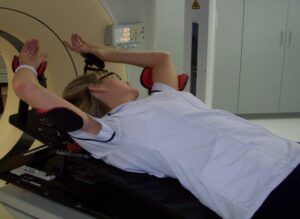
After having surgery it is often the case that arm mobility is affected. In radiotherapy we need patients who are having breast or chest wall radiotherapy to raise their arms above their heads for several minutes a day. Make sure you follow the physiotherapy exercises recommended by your team religiously after surgery to ensure you can comfortably complete your radiotherapy course. Also consider doing simple exercises around the house to improve your mobility, for example reaching to put cans on a high shelf. This will also help you maintain your mobility after you’ve finished your treatment(5).
Radiotherapy for Breast Cancer techniques
For some patients having radiotherapy to their left side, you may be asked to do a specific breathing technique to help minimise the dose to your heart(6). This can be a tricky technique to master so there are resources available to help prepare you prior to treatment.

To align you every day in the correct position, you may be asked to have permanent tattoos. These are tiny pin prick tattoos, typically placed on the left and right side of your rib cage and one centrally. These are used to ensure you are set up in exactly the right position each day for accurate, reproducible treatment. They will look different on different colour skin tones.
There is a newer technique called Surface Guided Radiotherapy (SGRT) which uses sophisticated 3D camera technology to accurately target and kill cancer cells. During your treatment, cameras monitor your exact position to make sure the radiation is precisely targeted. SGRT is often used to enable DIBH treatment for left-sided breast cancer with the benefit of minimising dose to the heart. SGRT means you don’t need to have any permanent markings(tattoos) made on your body, but be aware not all radiotherapy departments have this technology (7).
What to bring to radiotherapy appointments
If you are working, have caring responsibilities, or know that you struggle to get going in the mornings then please do ask the therapeutic radiographers for appointments to suit your circumstances. We cannot always accommodate your requests, but we will try!
The radiotherapy treatment itself is fairly quick and can take as little as 5 minutes and as long as 25 minutes. If you feel anxious during the treatment, why not consider bringing some music to play. Occasionally there may be delays for treatment, or if you are waiting for a specialist for a treatment review, so we advise that you bring something to take your mind off waiting, such as a book, phone/tablet or crochet/knitting pattern.
You may also want to bring a drink, some snacks and any medical information you may need e.g. list of medications or questions you want to ask. It can also be helpful to record your conversations with your oncologist or therapeutic radiographers if you know you struggle to retain information. It can sometimes feel overwhelming with the amount of information you are given but please don’t hesitate to ask staff to clarify anything you are unsure of or forgotten!
Many radiotherapy departments will have a designated website and many provide information about what to expect, so please do go on and have a look.
Ask to look at your radiotherapy treatment plan for Breast Cancer
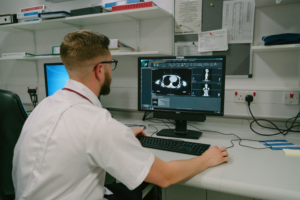
Although you may not be able to interpret your radiotherapy treatment plan, asking your therapeutic radiographers to go through it with you will show you where the radiation is actually targeting and will highlight where you are likely to get the effects of radiation. Every radiotherapy treatment plan is personalised to you and that is one of the reasons why everyone’s experience of radiotherapy side effects is different.
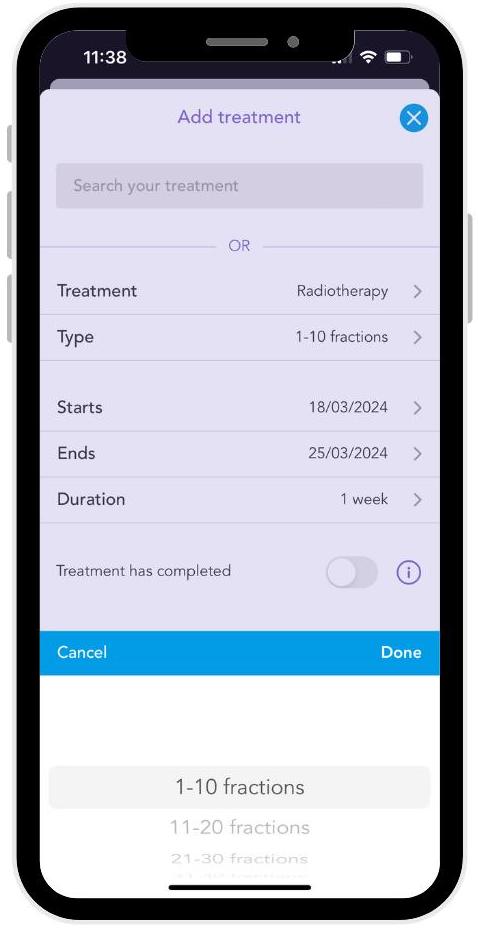 Did you know that you can add your radiotherapy treatment plan on the OWise app? Simply go to ‘Plan’, select radiotherapy treatment and choose how many fractions you have been prescribed. You can select your treatment start and end date then visualise your treatment plan as a chart or list.
Did you know that you can add your radiotherapy treatment plan on the OWise app? Simply go to ‘Plan’, select radiotherapy treatment and choose how many fractions you have been prescribed. You can select your treatment start and end date then visualise your treatment plan as a chart or list.
Radiotherapy skincare
Many patients will experience a radiotherapy skin reaction. This is not a sunburn, although it can have characteristics which are similar. Looking after your skin prior to, during and after radiotherapy will help. In our words at Rad Chat ‘moisturise, moisturise and moisturise’. Doing this will hydrate your skin, allow you to reconnect with your body, as well as help with any scars you may have. People always ask us what products to use, the evidence base is very limited and what we suggest is you use what you have always used on your skin, just be aware that you need to apply the cream right up the neck and under the armpit to ensure you cover the entire area.
Severe skin reactions are not normally seen due to advancements in radiotherapy treatment techniques. If you do notice a skin reaction, this will only be seen within the area you are being treated.(8). For patients with lighter skin tones, you might notice your skin within the treatment field may become pinker or redder. For patients with darker skin you may notice that the treatment area looks darker or more pigmented. Speak to the treatment therapeutic radiographers, or the treatment review team if you have any concerns or need some advice. Even when you have finished radiotherapy you may go on to experience skin reactions, which is totally normal, please do contact your radiotherapy team if you need advice and support.
Managing fatigue
Radiotherapy causes fatigue! This is not just feeling tired and it may surprise you that doing physical activity will actually help you manage fatigue(9). Personalise the activity for you. It does not have to be a gym session, it could be 10 minutes of hoovering. It does not have to be a run, it could be a gentle stroll. You know your body better than anyone else, so use that knowledge to pick the activity appropriate for you but try to keep active and get out of the house into nature if you can. We like to think of having physical activity snacks through the day, so when you are making a cup of tea could you sit and stand from a chair 10 times?
Listen to your body
Your body will go through a lot during your cancer treatment. It is okay to feel differently about your body after this. It is okay to be reluctant to consider being intimate with a partner. It is about finding your new normal, finding your comfort zone and loving your body how it is.
If you are struggling with body confidence there are many feel good workshops you can access through your local department. You can also speak to your local Boots about working with a a Boots Macmillan Beauty Advisor.
Sex, pleasure and intimacy can be important to people in different ways. It’s about taking things slowly and ensuring you are ready for this post treatment. Sometimes a conversation with your partner is all you need, or you may need specialist help and support in the form of a psychosexual specialist through your department.
Self-examination after breast cancer is very important as this will help you be more self-aware of your body and ensure you know how to feel for any further changes.
Use your Therapeutic Radiographers to support you through treatment
It can be easy to be a passive patient and just follow instructions blindly without asking why, or getting more information if you require it. Ask the therapeutic radiographers all the questions! We are experts in radiotherapy and so if you are not sure of what to do, or why, please do ask! Every patient is different, and you may not wish to know what is happening, or you may wish to know everything, we will be governed by you.
We are here to support you through your radiotherapy treatment and beyond. Within your radiotherapy department you will meet a wide range of therapeutic radiographers: for your initial appointment you might meet a consultant therapeutic radiographer who may consent you for treatment, a pre-treatment therapeutic radiographer who will help take your CT (planning) scan and may give you permanent tattoos if you need them.
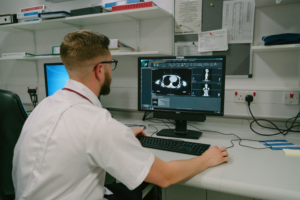
A dosimetrist or medical physicist will design your personalised radiotherapy treatment plan, and a treatment therapeutic radiographer who will deliver your treatment and answer any questions you have. You may also have a treatment review therapeutic radiographer who will be checking in on you during and after your radiotherapy. If you do not know who someone is, or what their role is within your treatment pathway is, please ask them!
Get information from the right sources

Did you know that you can add your radiotherapy treatment plan on the OWise app? Simply go to ‘Plan’, select radiotherapy treatment and choose how many fractions you have been prescribed. You can select your treatment start and end date then visualise your treatment plan as a chart or list.