
Bisphosphonates are commonly prescribed to women with breast cancer to treat bone thinning as many cancer therapies can weaken the bones. It has been demonstrated that the risk of fracture is increased in postmenopausal women with estrogen receptor (ER+) positive cancer who take aromatase inhibitors1, 2. Furthermore, bisphosphonates have also been studied to reduce the risk of breast cancer recurrence in the bone in early and secondary breast cancer3, 4.
How is bone loss measured? Tests like Dual Energy X-ray absorptiometry (DEXA) are performed to measure the bone mineral density (BMD) to quantify the calcium levels in your bones. This test is essential to diagnose osteoporosis or osteopenia. Osteopenia is the thinning of bone mass, while osteoporosis is the “fragile bone disease” caused by a deficiency in calcium, vitamin D, magnesium and other vitamins and minerals.
In this blog, we explore what bisphosphonates are and why they may be prescribed for early stage and secondary breast cancer. We also discuss how bisphosphonates work, and why dental hygiene and maintenance is important to be aware of whilst taking bisphosphonates.
What are bisphosphonates?
Bisphosphonates are drugs that target bone cells and help to prevent bone breakdown or fracture by making bones denser. They may be given orally or through injections. The most commonly prescribed bisphosphonates in breast cancer are zoledronic acid (Zometa®) and pamidronate (Aredia®). Although bisphosphonates can have many benefits, and have been an important treatment for many people, there are some rare risks to be aware of.
How do bisphosphonates exactly work?
 In order to understand how bisphosphonates work, we need to explain what an osteoclast is. An osteoclast is a type of bone cell that breaks down bone tissue5. Osteoclasts secrete acid and enzymes to break down proteins and the minerals within the bones. This breakdown process is called bone resorption, and it is very important for bone maintenance, repair and remodelling.
In order to understand how bisphosphonates work, we need to explain what an osteoclast is. An osteoclast is a type of bone cell that breaks down bone tissue5. Osteoclasts secrete acid and enzymes to break down proteins and the minerals within the bones. This breakdown process is called bone resorption, and it is very important for bone maintenance, repair and remodelling.
Bisphosphonates prevent bone resorption from happening by killing osteoclasts6. This way, osteoclasts cannot do their job and bone density is increased.
Bisphosphonates and breast cancer
a) Help reduce the risk of cancer in early breast cancer
Bisphosphonates such as zoledronic acid are usually given to patients with higher risk of the cancer coming back who are:
- Postmenopausal, or
- Have had therapy to stop their ovaries (goserelin (Zoladex®)) from producing oestrogen7.
Research has shown that after 10 years, postmenopausal women with early breast cancer who were on bisphosphonates had reduced risk of:
- breast cancer recurrence (by 3.3%),
- cancer coming back to the bone (by 2.2%)
- and all-cause of death (by 2.3%)3.
However, it is important to note that these benefits were not observed in premenopausal women3, 4.
b) In secondary breast cancer for those with bone metastases
In breast cancer, the bone is the main site where cancer cells can spread to (metastasis) and this can cause considerable side effects including fractures, severe pain, nerve compression and hypercalcaemia. Bisphosphonates may be taken by those with secondary breast cancer with bone metastases to treat pain and reduce the risk of fracture, as well as a preventative measure to stop initial or further metastatic spread. In fact, a systematic review and meta-analysis of nine studies that included over 2,800 patients with breast cancer with bone metastases showed that bisphosphonates reduced the risk of a skeletal-related event (SRE) by 15% and also delayed the time to a SRE. In six out of eleven studies, treatment with bisphosphonates also significantly improved bone pain8.
“In breast cancer, drugs that block bone breakdown are a proven therapy when bone metastases are present, reducing fractures, pain and the requirement for surgery and radiation.” – Dr. Julie Gralow, new chief medical officer for ASCO.
Also, it has been hypothesised that bisphosphonates could reduce the spread of bone metastasis as excess osteoclast (bone cell) activity could help the tumour metastases to survive. However, this is still controversial and clinical trials have found mixed results 9, 4.
It is important to note that bisphosphonates can come with an array of side effects which we discuss below, so this treatment option should be discussed with your care team.
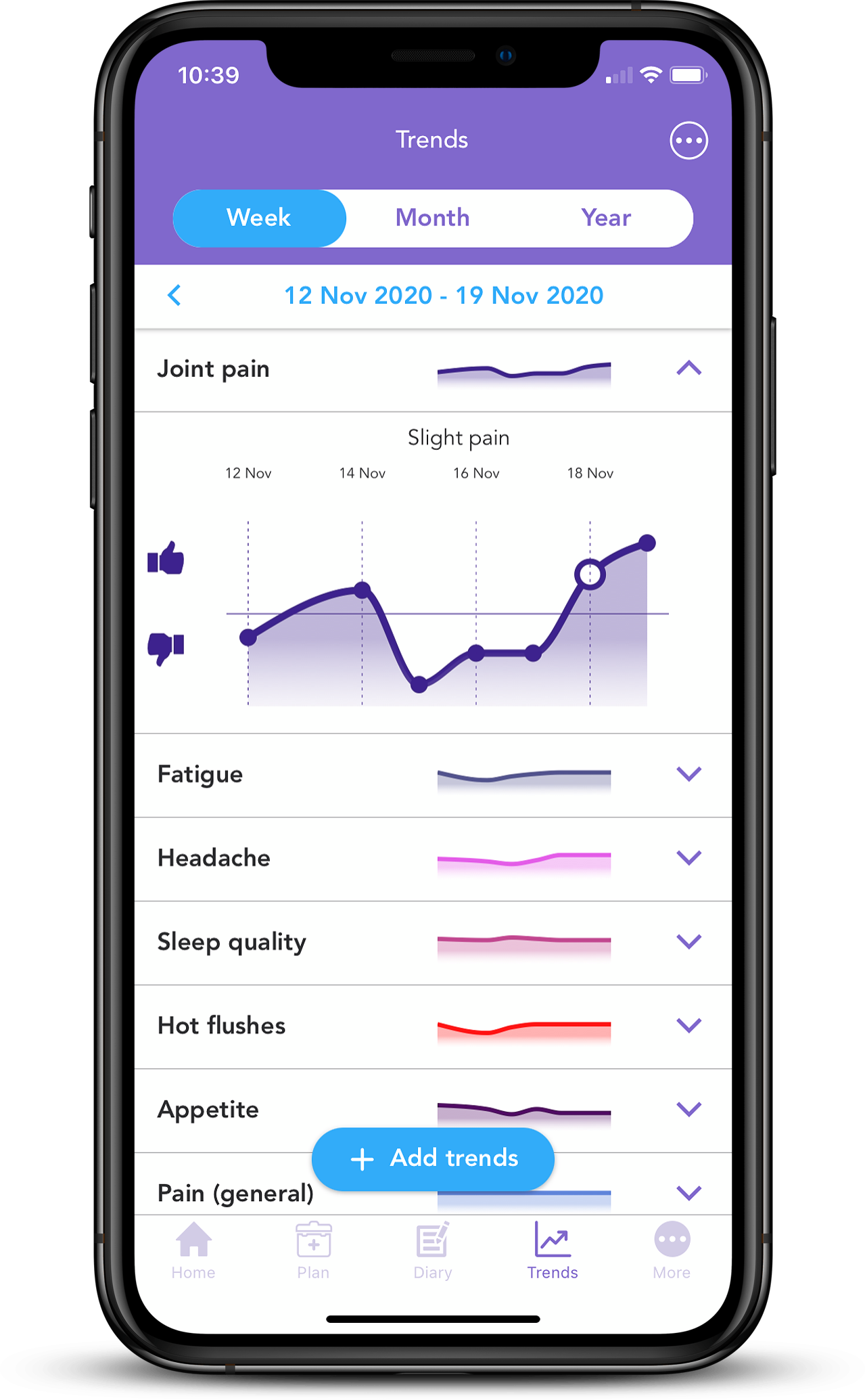
With the free OWise Breast Cancer app, you can keep an overview of all of your treatments in a chronological graph and list format. You can also manually add any treatments that are not in the list by selecting “Other”. In addition, you can add appointments, notes, photos and contacts all in one place.
c) Help to keep bones strong when undergoing treatments that have bone thinning effects
As mentioned previously, bisphosphonates are commonly prescribed to women with breast cancer to treat bone loss as many cancer therapies can weaken them. Your doctor may prescribe them depending on the results from your bone mineral density test.
Why is dental hygiene/maintenance important to be aware of whilst taking bisphosphonates?
a) Osteonecrosis of the jaw
Although rare, bisphosphonate-related osteonecrosis of the jaw (BROJ) is a serious, possible side effect of bisphosphonate treatment.
What is osteonecrosis of the jaw?
Osteonecrosis of the jaw is when the cells in the jaw bone begin to die. Symptoms include:
- severe pain
- swelling
- a numb jaw
- loose teeth
- visible bone in the mouth
It has been estimated that BROJ incidence in breast cancer patients taking bisphosphonates is approximately 3 out of 100 people10. Similarly, a 3 year longitudinal study investigating BROJ in a variety of advanced cancer patients reported an incidence rate ranging from 0.08% at the first year of treatment to 2.8% after the third year of treatment, with the lowest rates in breast cancer patients (2.4%)11.
For some people, bisphosphonates treatment and other risk factors including dental procedures, such as dental surgery, tooth extractions or dental implants may lead to BROJ.
“We’re much more cautious about using them when the risk of breast cancer recurrence is low and the risk of osteonecrosis of the jaw (ONJ), for example, is elevated, as in smokers and those with poor dental health.” – Dr. Poorni Manohar, physician-researcher with the Hutch and SCCA.
It is important to understand the risks before you start treatment, to let your oncologist know about your dental history and to inform your dentist that you plan to start taking bisphosphonates. Certain treatments may be adapted or you may be recommended to complete dental work before you start bisphosphonate treatment.
b) How to minimise the risk of BROJ: dental care
It is important that your care team know of any past, current and future dental work and dental work plans as they can cause damage and ‘trauma’ to the mouth area. This can increase the risk of developing BROJ because, as previously discussed, bisphosphonates stop bone resorption (check the “How do bisphosphonates exactly work?” section). Bone resorption plays a key role in bone maintenance, repair and remodelling which may need to take place after dental work.
Before starting bisphosphonates treatment, schedule a dental exam and inform your dentist that you will be starting bisphosphonates treatment. Discuss if you have any heightened risk due to your personal dental health. The exam is important as it will reveal if any dental work needs to be completed before the start of treatment and will allow your care team to gain insight on your dental health before treatment starts. Your dentist may also conduct an x-ray of your jaw which can be used to refer back to during and after treatment to see if there have been any changes to your dental health.
Dental hygiene is key for minimising the risk of BROJ. Schedule a dental cleaning before you start treatment and regularly throughout treatment. Daily dental hygiene (flossing, mouthwash and thorough brushing after each meal) will prevent bacterial overgrowth and infections that can lead to osteonecrosis. Giving up smoking is recommended to reduce risk of irritating and infecting the mouth. In fact, a bisphosphonate study reported higher incidence of BROJ in smokers11. If you notice any bleeding or develop any pain, contact your dentist immediately.
c) Are there any other potential side effects?
Besides osteonecrosis of the jaw, there are other side effects associated with bisphosphonates. The risk of these side effects may increase as dose and overall treatment length increases.
Hypocalcemia
As bisphosphonates reduce bone resorption there is a risk of developing hypocalcemia. Hypocalcemia is low levels of circulating calcium. This can manifest as feeling sluggish and can develop to bone and muscle pain and more serious conditions such as tetany which causes muscle spasms12,13. Before starting and during treatment your doctor will check your calcium levels to ensure they are normal. To reduce the risk of hypocalcemia your doctor may prescribe calcium and vitamin D supplements14,15.
Kidney damage
Bisphosphonates are not fully metabolized/broken down by the kidneys and can thus cause kidney damage. Your care team will monitor kidney function throughout treatment. Hydration is key to support kidney function and reduce risk of damage.
Pregnancy, breastfeeding and bisphosphonates
Little is known of the effects and safety of bisphosphonates during pregnancy and breastfeeding. However, as bisphosphonates can pass the blood-uterine barrier (entering the baby’s environment) and are present in breast milk, it is recommended to stop bisphosphonate treatment before pregnancy until after breastfeeding. If you are planning on a pregnancy, are pregnant or breastfeeding please consult with your care team.
Bisphosphonates can cause other side effects including:
- Whiter vaginal discharge, this is not harmful16
- Flu symptoms
- Headaches
- Nausea
- Indigestion
We hope that you now better understand what bisphosphonates are, how they work and the importance of dental care throughout treatment. Our aim is to make sure you are always kept informed so make sure to follow our Instagram and Twitter accounts for any updates.
If you would like to start monitoring and tracking your treatment side effects, you can download the FREE OWise app from the iOS App Store or Google Play Store.
References
- Brufsky, Adam, et al. “Zoledronic acid inhibits adjuvant letrozole–induced bone loss in postmenopausal women with early breast cancer.” Journal of Clinical Oncology 25.7 (2007): 829-836.
- Hadji, Peyman, et al. “Management of Aromatase Inhibitor-Associated Bone Loss (AIBL) in postmenopausal women with hormone sensitive breast cancer: Joint position statement of the IOF, CABS, ECTS, IEG, ESCEO, IMS, and SIOG.” Journal of bone oncology 7 (2017): 1-12.
- Early Breast Cancer Trialists’ Collaborative Group. “Adjuvant bisphosphonate treatment in early breast cancer: meta-analyses of individual patient data from randomised trials.” The Lancet 386.10001 (2015): 1353-1361.
- https://www.nice.org.uk/advice/es15/chapter/key-points
- Kylmaoja, Elina, Miho Nakamura, and Juha Tuukkanen. “Osteoclasts and remodeling based bone formation.” Current stem cell research & therapy 11.8 (2016): 626-633.
- Drake, Matthew T., Bart L. Clarke, and Sundeep Khosla. “Bisphosphonates: mechanism of action and role in clinical practice.” Mayo Clinic Proceedings. Vol. 83. No. 9. Elsevier, 2008.
- Gnant, M., et al. “S1-2: Long-Term Follow-Up in ABCSG-12: Significantly Improved Overall Survival with Adjuvant Zoledronic Acid in Premenopausal Patients with Endocrine-Receptor–Positive Early Breast Cancer.” (2011): S1-2.
- Wong, Matthew HF, Martin R. Stockler, and Nick Pavlakis. “Bisphosphonates and other bone agents for breast cancer.” Cochrane database of systematic reviews 2 (2012).
- Brufsky, Adam, and Aju Mathew. “Bisphosphonates, bone, and breast cancer recurrence.” The Lancet 386.10001 (2015): 1319-1320.
- Varun, B. R., et al. “Bisphosphonate induced osteonecrosis of jaw in breast cancer patients: A systematic review.” Journal of oral and maxillofacial pathology: JOMFP 16.2 (2012): 210.
- Van Poznak, Catherine H., et al. “Association of osteonecrosis of the jaw with zoledronic acid treatment for bone metastases in patients with cancer.” JAMA oncology 7.2 (2021): 246-254.
- Prommer, Eric E. “Toxicity of bisphosphonates.” Journal of palliative medicine 12.11 (2009): 1061-1065.
- Domschke, Christoph, and Florian Schuetz. “Side effects of bone-targeted therapies in advanced breast cancer.” Breast Care 9.5 (2014): 332-336.
- Tanvetyanon, T., and P. J. Stiff. “Management of the adverse effects associated with intravenous bisphosphonates.” Annals of Oncology 17.6 (2006): 897-907.
- Kreutle, Veronika, et al. “Bisphosphonate induced hypocalcaemia–report of six cases and review of the literature.” Swiss medical weekly 144.2526 (2014).
- “Vaginal Discharge: A Side Effect of Treatment.” Breastcancer.org, 26 Apr. 2019, www.breastcancer.org/treatment/side_effects/vaginal_discharge.
